Office of Research & Development |
 |

VA Research Currents archive
Posted July 16, 2013
(Summer 2013 VA Research Currents)
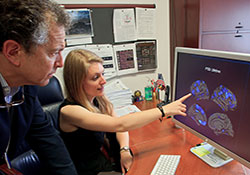
Dr. William Milberg and Emily Lindemer examine brain MRI images. The scientists are with VA's Boston-based Translational Center for TBI and Stress Disorders. (Photo by Thomas Manders)
A study by researchers at the VA Boston Healthcare System offers an in-depth look at the effects of combat and other traumas on the brain. The findings are now online in the journal NeuroImage: Clinical.
The study included 104 Veterans who served in Iraq or Afghanistan. The researchers focused on the effects of posttraumatic stress disorder on the cerebral cortex—the outermost layer of the brain. Known as the brain's "gray matter," the cortex, two or three millimeters thick, plays a key role in memory, attention, and other mental tasks. The cortex loses thickness with normal aging, and research on many brain conditions has generally linked thinning of the cortex to reduced cognitive function.
The study found that both current PTSD and a person's "lifetime burden" of PTSD, or trauma exposure, are associated with reduced thickness in various areas of the cortex. The findings were based on two MRI brain scans of each study volunteer.
"We believe this is the first study to show clearly the burden of psychological trauma across the lifespan, and to relate this burden to the thickness of the cortex across the entire brain," says lead author Emily Lindemer, an investigator with VA's Translational Center for TBI and Stress Disorders (TRACTS).
Senior authors on the study were TRACTS director Regina McGlinchey, PhD, and co-director William Milberg, PhD. Both are also with Harvard Medical School. David Salat, PhD, with TRACTS and the Martinos Center for Biomedical Imaging, also worked on the study.
The TRACTS team also looked at how traumatic brain injury compounds the cortical damage. They found "more marked reductions in cortical thickness" when Veterans with PTSD also had a history of at least one traumatic brain injury, in some cases from a blast.
Several past studies have linked PTSD to reduced volume in various brain areas. These include the hippocampus and amygdala, as well as the anterior cingulate, which is part of the cortex. But findings overall have been mixed. And researchers still aren't sure if PTSD causes these brain changes, or if smaller volume in certain brain structures is a pre-existing risk factor for PTSD.
The new study doesn't answer the question directly. But it does suggest that the longer a person lives with PTSD, the more pronounced the effects on the cortex. "The longer an individual lives with a trauma-related psychological burden, the greater the observed reduction in [cortical] thickness will be," wrote Lindemer and colleagues. They also observed that reductions in thickness were spread across more areas of the cortex in those Veterans who had a longer history of PTSD or trauma exposure. In fact, most Veterans in the study reported having experienced at least one trauma prior to their combat deployment.
According to the researchers, the results show the importance of considering trauma across the lifespan, and not just "a single snapshot of current PTSD symptoms," when trying to understand trauma's effects on the brain.
The study was part of ongoing VA-funded research at TRACTS exploring the effects on the brain of combat-related brain injuries, both physical and emotional. To watch a video on the center's work, visit www.research.va.gov/news/features/tracts.cfm.