Office of Research & Development |
 |
Dementia is a general term for a range of medical conditions involving a decline in memory, thinking, judgment, and learning severe enough to impair daily life. Dementia is not a disease by itself.
Alzheimer's disease, first described by Alois Alzheimer in 1906, is one of the most common forms of dementia. Alzheimer's accounts for 60% to 80% of all diagnosed dementia cases. It is a progressive disease that involves the deterioration of nerve cells in the brain, which in turn affects thoughts, memory, and language.
People with Alzheimer's disease may at first notice mild confusion and difficulty remembering things. Eventually, affected people may fail to recognize their surroundings or important people in their lives, and some undergo dramatic personality changes. Alzheimer's is the sixth leading cause of death in the United States—usually resulting from secondary infections, like pneumonia, that are common in incapacitated patients.
Existing medications and management strategies may help to improve Alzheimer's symptoms, allowing people with the diagnosis to maximize their ability to function and maintain their independence for a while. At present, however, there is no cure for Alzheimer's disease.
VA provides care for Veterans with Alzheimer's disease and other forms of dementia throughout the full range of VA health care services. Among the services VA provides to eligible Veterans are home-based primary care, homemaker and home health aides, respite care, adult day health care, outpatient clinic services, inpatient hospital services, nursing home services, and hospice care. VA also provides support for caregivers.
VA's Geriatric Research Education and Clinical Centers (GRECCs) were established in 1975 to increase basic knowledge of aging and diseases that affect an older population and to improve the health of aging Veterans. VA operates 20 GRECCs located throughout the United States. They are tasked with three aims: to increase knowledge of geriatric care through research, to improve health care for older Veterans through innovation, and to provide training and education on clinical care for older adults.
VA researchers seek to understand and address the causes of Alzheimer's disease. Some areas of focus for Alzheimer's research are potential drug therapies, genetic and environmental causes, and long-term care models for patients. Still other researchers are working to better understand the connection between Alzheimer's and chronic diseases like diabetes.
In addition to these avenues of research, VA investigators are also looking at ways to support and nurture family members who care for Veterans with Alzheimer's disease in their own homes.
VA has partnered with the National Institutes of Aging (NIA) to improve overall health for aging Veterans and to increase participation in Alzheimer's disease clinical trials. In 2021, VA investigators launched a pilot program that successfully recruited more than 60 Veterans for research on Alzheimer's disease and related dementias. As part of the program, VA and NIA have partnered with the NIA-funded Alzheimer's Disease Research Centers (ADRCs) to increase Veteran participation in targeted clinical trials.
VA is working with NIA to develop an Alzheimer's Disease Recruitment Network, form stronger relationships between national and local research agencies, and investigate unique risk factors for Veterans with Alzheimer's and related dementias.
For more information about neurological disorders, visit our Multiple Sclerosis, Parkinson's disease, Spinal Cord Injury, and Traumatic Brain Injury topic pages.
If you are interested in learning about joining a VA-sponsored clinical trial, visit our research study information page.
Neuroimaging Initiative—The Alzheimer's Disease Neuroimaging Initiative (ADNI) was established in 2004 to find new ways to diagnose and predict the onset of Alzheimer's disease. VA researcher Dr. Michael Weiner is founder and principal investigator for ADNI. Weiner is affiliated with the VA-University of California Center for Imaging of Neurodegenerative Diseases located at the San Francisco VA Health Care System.
The $67 million initiative—funded by the National Institute on Aging and other partners—seeks to identify brain changes linked to Alzheimer's disease. The funds are administered by a VA nonprofit corporation, the Northern California Institute for Research and Education (NCIRE). The program is coordinated by the Alzheimer’s Therapeutic Research Institute (ATRI) at the University of Southern California. ADNI is now in its third phase, in which researchers are working to validate biomarkers for Alzheimer's disease clinical trials. ADNI-3 began in 2016 and will run through 2021.
ADNI-1 researchers found that people with Alzheimer's disease can have high levels of a protein called beta-amyloid 42 in their brains. While dementia can result from any number of health problems, such as strokes, amyloid buildup happens only in patients with Alzheimer's. At present, amyloid levels can be determined only through spinal taps or special diagnostic imaging.
The team developed a simple blood test that could potentially be used to predict the buildup of amyloid in the brain with modest accuracy. The 2015 study suggested that blood-based biomarkers have the advantage of being safe, affordable, and easy to administer to participants in large clinical trials. Such a test could improve clinical care for patients, who would benefit from early treatment for Alzheimer's disease.
Cellular stress can contribute to Alzheimer’s disease—A type of cellular stress called cellular senescence, known to be involved in cancer and aging, has been implicated in Alzheimer’s disease. Researchers at the South Texas Veterans Health Care System and the University of Texas identified cellular senescence in brain tissue taken after death from Alzheimer’s disease patients and deceased patients who had supranuclear palsy, in a 2018 study.
To investigate the effects of cellular senescence, the team used genetically modified mice that had tau proteins and cognitive deficits similar to people with Alzheimer's disease. They used a combination of drugs to clear senescent cells from the tau mice. After treatment, they found the mice's brain structure and functioning had improved.
Researchers used drugs that targeted and killed only senescent cells. They hope to begin pilot studies in humans soon, and also to study whether cellular senescence is present in traumatic brain injury.
Cellular senescence is associated with harmful tau protein tangles in the brain that are involved with many diseases, including Alzheimer’s and traumatic brain injury. Senescence allows stressed cells to survive, but these cells may function abnormally and secrete substances that kill surrounding cells.
Clumps of protein contain genetic material in Alzheimer's patients—A 2021 study by researchers with the Central Arkansas Veterans Healthcare System and the University of Arkansas found that protein aggregates in patients with Alzheimer’s disease include more than just protein. The clumps of protein also contain specific genetic material (DNA and RNA) pulled into aggregates, either by the proteins that bind them or in the course of creating new proteins—a process known as protein synthesis. The research team also found that slowing the process of protein synthesis can remove almost all of the RNA from aggregates.
The study provides the first evidence that RNA and DNA sequences are found in protein aggregates that are specific to individual diseases. Their overabundance in aggregates specific to Alzheimer’s disease suggests these aggregates play a role in causing the disease, and in determining which individuals may be more susceptible to developing it.
Proteins are amino acids that join together to form long chains, and help repair and build body tissues, keep immune systems strong, and coordinate bodily functions. Protein aggregation involves clumps of proteins that can cause injury or death to cells. It is a common characteristic of neurodegenerative disease. Protein aggregates are associated with most diseases that happen as people age, including Alzheimer’s disease.
Mechanism behind rare dementia uncovered—Frontotemporal dementia (FTD) is a group of disorders caused by nerve damage in the frontal and temporal lobes of the brain. It is the second most common cause of dementia in people under age 65. FTD destroys regions of the brain that control personality, behavior, and speech. There is currently no treatment for the disorder.
In 2020, researchers at the San Francisco VA Health Care System and the University of California published a study that examined age-related changes in the thalamus, a region of the brain that controls motor and sensory signals. The team looked at mouse brains to see how gene expression changes as the animals age. Their work showed how a common human FTD mutation could cause DNA-binding protein 43 to build up in the brain. The mutation also drives diseased microglial cells to kill vulnerable neurons in the thalamus.
Microglial cells, when healthy, remove damaged neurons in the central nervous system and are a type of cell that is the primary line of immune system defense for the brain and spinal cord. The team is now working to identify drugs that could make diseased microglial cells healthy again and potentially protect the brains of patients with FTD.
Biomarkers helpful in identifying Alzheimer's disease—Biological measures of brain health can be useful in identifying clinical Alzheimer's-type dementia (CATD), according to 2020 review study by the Minneapolis VA Health Care System and the University of Minnesota. Currently, the only way to confirm Alzheimer's disease is to conduct an autopsy of the brain following death. The research team examined the efficacy of two different types tests—brief cognitive assessments and clinical biomarkers—for distinguishing Alzheimer's disease and other causes of dementia in living people.
The researchers found cognitive assessments were highly accurate in identifying CATD, but were less accurate in distinguishing mild cognitive impairment (MCI) from CATD.
The biomarker tests included amyloid PET (positron emission tomography) scans, which map the build-up of amyloid protein; fluorodeoxyglucose (FDG)-PET scans, which map how the brain absorbs glucose; and MRI (magnetic resonance imaging) testing, which detects changes in the temporal lobe of the brain, including the hippocampus. The team also assessed single-photon emission computed tomography (SPECT) and cerebral spinal fluid (CSF) testing. The first three tests provided dementia diagnoses that were more than 90% accurate.
According to the research team, more accurate diagnoses of dementia in living patients can help direct clinical decision making on the best treatments for individuals. More accurately identifying different types of dementia can also help direct patients to clinical trials.
Women Veterans with alcohol use disorder are at increased risk of dementia—A 2021 study by researchers at the San Francisco VA Medical Center and University of California compared the records of more than 2,200 women Veterans who were 55 years or older and had alcohol use disorder with those of a control group. The researchers found that study participants who had alcohol use disorder were more than three times as likely to develop dementia than those who did not. Eighty-two women Veterans in the study developed dementia.
The team concluded alcohol use, especially alcohol use disorder, should be considered when evaluating patient risk for dementia. They also believe that programs and services to address the growing problems of alcohol use disorder and dementia in older women would be beneficial.
Agent Orange exposure and dementia—A 2021 study found that Vietnam-era Veterans with Agent Orange exposure were nearly twice as likely as those without to receive a dementia diagnosis, even after adjusting for other variables.
Researchers at the San Francisco VA Health Care System found that 5% of Veterans with a documented exposure to Agent Orange were diagnosed with dementia, compared with 2.5% of Veterans with no known exposure. The team also learned that exposed Veterans were diagnosed an average of 15 months earlier than non-exposed Veterans.
The team reviewed the medical records of over 300,000 Vietnam Veterans who received care in VA from Oct. 1, 2001, through Sept. 30, 2015. They made statistical adjustments to account for variables—for example, Veterans with Agent Orange exposure were more likely to be diagnosed with PTSD or traumatic brain injury. Despite this, the additional risk remained.
The researchers suggest that additional studies be conducted to determine the relationship between Agent Orange exposure and dementia, and hope their findings will encourage early screening.
Brief cognitive assessments may be useful in diagnosing Alzheimer's—Clinicians use a number of tests to identify cognitive (thinking) impairments related to Alzheimer's disease. In 2020, researchers with the Minneapolis VA Health Care System and the University of Minnesota conducted a review on the accuracy of brief cognitive assessments used to distinguish Alzheimer's-type dementia from mild cognitive impairment or normal cognition.
Fifty-seven studies met the team's criteria. The team found several of these tests could differentiate between moderate-to-advanced Alzheimer's disease and normal cognition. However, the tests were less able to distinguish between mild Alzheimer's and mild cognitive impairment, or between mild cognitive impairment and normal cognition.
The team hopes that effective tests may help providers decide which patients warrant a more comprehensive diagnostic evaluation. They may also provide a less burdensome way to document cognitive impairment when patients have already undergone an assessment and show evidence of functional impairment.
Using spectroscopy to detect Alzheimer’s—Researchers with the VA Bedford and Boston health care systems developed technology that uses light to detect structural changes in the brain related to Alzheimer’s disease, in a 2021 study.
Spectroscopy measures how light is scattered and absorbed when passing through matter. The technology works by positioning two fiber-optic probes on the surface of a patient’s temple. One probe delivers near-infrared light non-invasively and harmlessly into the patient’s brain. The other probe collects the light that scatters back.
Using a computer algorithm, the researchers identified two spectral features that signaled the difference between patients with late-stage Alzheimer’s from controls with normal brain function. A minor adjustment to those two features allowed them to classify patients with mild cognitive impairment according to degree of impairment. The technique could become a simple, completely non-invasive method of early Alzheimer’s detection, and also has potential as a way to assess the effectiveness of treatment.
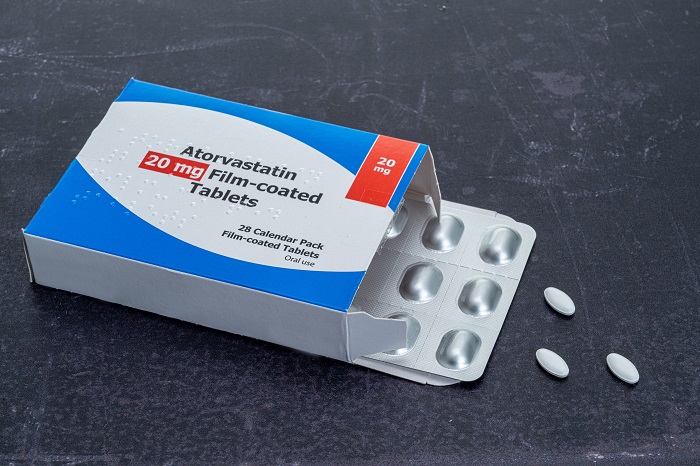
High LDL cholesterol linked to early-onset Alzheimer's—Low-density lipoprotein (LDL) cholesterol may play a causal role in the development of early-onset Alzheimer's disease, according to a 2019 study. The results could help clinicians better understand how Alzheimer's develops, said researchers with the Atlanta VA Medical Center and Emory University.
About 10% of all Alzheimer's cases are early-onset, appearing in patients younger than age 65. The research team looked at the genomes of 2,125 people, 654 of whom had early-onset Alzheimer's. They found that participants with elevated LDL levels were more likely to have early-onset Alzheimer's. The team did not find a link between Alzheimer's and high-density lipoprotein (HDL) cholesterol, and only a very slight association with triglyceride levels.
The researchers suggest more research is needed to fully explain the connection between Alzheimer's disease and cholesterol. They noted that the relative rarity of early-onset Alzheimer's disease presents a challenge in finding enough samples to perform large genetic studies.
Anticholinergic drugs are associated with cognitive decline—A class of drugs called anticholinergics may be associated with an increased risk of cognitive decline, especially in older adults at greater risk of Alzheimer's disease. These drugs are typically used for a broad array of conditions, from allergies and colds to hypertension and urinary incontinence.
The 2020 study was led by researchers at ADNI and the University of California San Diego. The team found that participants with normal thinking who were taking at least one anticholinergic drug at the beginning of the 10-year study period were 47% more likely to develop mild cognitive impairment than those who were not. Anticholinergic drugs work by blocking acetylcholine, which is a type of neurotransmitter or chemical messenger known to be critical for memory function.
There were 688 adults in the study, evenly divided by sex, with an average age of 74. None of the participants displayed cognitive or memory problems at the beginning of the study, and all were given annual comprehensive cognitive tests for up to 10 years.
The research team noted that more work is needed to examine the cognitive effects of anticholinergic medications and to determine if these medications accelerate age-related cognitive changes.
Diabetes and Alzheimer's combined are linked to greater cognitive decline—Patients with both diabetes and Alzheimer's risk factors showed greater cognitive decline than those with risk factors for only one condition, found a 2020 study by researchers at the VA San Diego Healthcare System.
The team followed the cognitive functioning of more than 800 Veterans for five years, and found that patients with both diabetes and at least one Alzheimer's risk factor showed the most cognitive decline over that period, compared to people without both risk factors.
Risk factors for Alzheimer's included subtle cognitive decline, genetic risk, and three biomarkers that are found in spinal fluid. The study results suggest that diabetes interacts with Alzheimer's risk factors to increase cognitive decline.
Prevalence of polypharmacy in older adults with dementia—One in seven people with dementia who live in the community are taking at least three medicines (polypharmacy) that act on the central nervous system (CNS), according to a 2021 study by researchers from the VA Ann Arbor Health Care System and the University of Michigan. Older adults who take three or more CNS-active medicines are at greater risk of memory problems, falls, and death, according to the researchers.
The study looked at data from 1.2 million people with dementia and focused on medications such as antidepressants, sedatives used as sleep medications, opioid painkillers, antipsychotics, and anti-seizure medications. The team said regular prescription drug reviews could help spot risky drug combinations.
Gene suppression may protect against Alzheimer’s disease—Eliminating a gene called MSUT2 (mammalian suppressor of tauopathy 2) shows promise in preventing the development of Alzheimer’s disease, according to a 2018 study.
Researchers from the South Texas Veterans Health Care System in San Antonio and the University of Texas Health Science Center deleted the MSUT2 gene in genetically modified mice that have an overabundance of tau (PS19), a protein that causes Alzheimer's disease in humans. The PS19 knock-out mice showed decreased levels of tau tangles and had fewer learning and memory problems.
Previous studies have shown that abnormal levels of tau in the brain correlate strongly with cognitive decline in Alzheimer’s disease patients. The team believes that if MSUT2 can be targeted by drugs, this would provide a new approach for treating Alzheimer’s and related disorders.
Preventing seizures after a brain injury can alleviate dementia—Researchers with the Pittsburgh VA Healthcare System, the University of Alberta, and other institutions published a 2021 study that found blocking seizures after head injuries can slow or prevent the onset of dementia.
The team exposed genetically modified zebrafish to traumatic brain injury (TBI) via pressure waves. After the procedure, many zebrafish showed dementia-like behavior and seizures. The team then assessed the level of abnormal tau proteins in the zebrafishes' brains using florescent light. Their results showed that posttraumatic seizures are linked to abnormal tau levels following TBI.
The team also found that anti-convulsant drugs can lower high levels of tau proteins in the brain—one of the causes of Alzheimer’s disease—and can potentially alleviate dementias associated with TBI.
Experiencing seizures after TBI is a major risk factor for certain types of dementia, including Alzheimer’s disease and chronic traumatic encephalopathy. Neurologists often prescribe anti-epileptic medications to prevent seizures in patients who have suffered TBIs.
The researchers suggested that refining the use of current anti-epileptic treatments can better prevent seizures and potentially stop dementia from developing later in life.
Gene therapy in mice preserves learning and memory—Gene therapy prevented learning and memory loss in a mouse model of Alzheimer’s disease, in a 2021 study by investigators with the VA San Diego Healthcare System, the University of California, and other institutions.
Introducing a therapeutic compound to a precisely targeted region of the brain may restore or protect normal brain function, and even reverse the process of degeneration. The researchers used a harmless viral vector to introduce synapsin-Caveolin-1 cDNA into the hippocampus region of three-month-old mice that were genetically modified to exhibit learning and memory deficits as they got older. (The hippocampus is a region of the brain that plays a major role in learning and memory.)
The team found learning and memory in these mice were preserved after receiving the compound, suggesting that this type of gene therapy could restore brain plasticity (the ability of the brain to change and adapt ) and improve brain function in people with Alzheimer’s disease and other forms of neurodegeneration. The investigators hope to advance their work to human clinical trials soon.
Enzyme modulation may prevent Alzheimer's disease—Researchers at the VA San Diego Healthcare System, the University of California San Diego, and Massachusetts General Hospital have identified new drugs that could prevent Alzheimer's disease by modulating a key enzyme involved in forming amyloid plaques in the brain. The drugs, known as γ-secretase modulators, slightly alter the activity of γ-secretase enzymes so that they produce fewer Aβ peptides, which are prone to form plaques in the brain.
Previous efforts to inhibit γ-secretase enzymes have proven to be unsafe in humans, because the enzymes, along with β-secretase enzymes, also have functions that are important for proper brain functioning.
In the 2021 study, the research team reported they had tested a drug that modulates γ-secretase enzymes in rodents, monkeys, and macaques, and found that it decreased plaque formation and inflammation thought to contribute to Alzheimer's disease.
If human clinical trials are successful, the drug could be used to prevent Alzheimer's in patients with genetic mutations that increase disease susceptibility or in cases where amyloid plaques have already been detected.
rTMS reduces apathy in Alzheimer's patients—A 2020 study found that brain stimulation therapy can improve apathy in Alzheimer's patients. The study was led by researchers at the Central Arkansas Veterans Healthcare System. Apathy involves loss of motivation, as well as social withdrawal, and is the most common behavioral problem in people with Alzheimer's disease.
Repetitive transcranial magnetic stimulation (rTMS) involves applying magnetic coils to specific points on the scalp to create an electrical current in brain cells. The technology is being studied widely for a number of brain disorders.
The research team found significantly greater improvement in apathy levels for study participants who received rTMS compared to the control group. The effect lasted for up to three months. The team concluded that rTMS may be safely used in people with Alzheimer's disease and may improve apathy, function, and some aspects of cognition.
Water-based therapy enhances Veteran recall—Researchers at the VA Palo Alto Health Care System are examining the effectiveness of a water-based exercise program combined with cognitive training to improve mild cognitive impairment.
The study, called WATER-VET, includes 50 Veterans with mild cognitive impairment who will take part in a six month water-based exercise training program that emphasizes cardiovascular fitness and strength training through a combination of non-weight bearing exercises. It will be followed by classroom-based cognitive training.
The team hopes to find evidence for using water-based training as an effective way to augment cognitive training. Future plans include conducting a full-scale clinical trial to examine nondrug therapies to treat mild cognitive impairment.
Increased risk of dementia in older female US veterans with alcohol use disorder. Bahorik A, Bobrow K, Hoag T, Yaffe K. Alcohol use disorder among female Veterans aged more than 55 years appears to be associated with a more than threefold increase of dementia. Addiction. 2021 Aug;116(8):2049-2055.
Near-infrared optical spectroscopy in vivo distinguishes subjects with Alzheimer’s disease from age-matched controls. Greco FA, McKee AC, Kowall NW, Hanlon EB. Near-infrared spectroscopy can detect and classify diseased and normal human brain in vivo. J Alzheimers Dis. 2021 Jun;82(2):791-802.
MRI-assessed locus coeruleus integrity is heritable and associated with multiple cognitive domains, mild cognitive impairment, and daytime dysfunction. Elman JA et al. Magnetic resonance imaging of the locus coeruleus brain region could aid in early detection of Alzheimer's disease. Alzheimer's Dement. 2021 Jun;17(6):1017-1025.
Drivers of long-term care considerations by persons with cognitive impairment. Shepherd-Banigan M, James HJ, Smith VA, Plassman BL, Jutkowitz E, Belanger E, Van Houtven CH. Perceived financial constraints limit the range of choices in long term care (LTC) planning. By understanding which factors drive patients to consider each type of care, clinicians can guide patients and their families in LTC planning. J Appl Gerontol. 2021 Jun;40(6):648-660.
“Protein aggregates” contain RNA and DNA, entrapped by misfolded proteins but largely rescued by slowing translational elongation. Shmookler Reis RJ, Alturi R, Balasubramaniam M, Johnson J, Ganne A, Ayyadevara S. Co-translational misfolding of nascent proteins may ensnare polysomes into aggregates, accounting for most of their RNA content. Aging Cell. 2021 May;20(5):e13326.
Agent Orange exposure and dementia diagnosis in US Veterans of the Vietnam era. Martinez S, Yaffe K, Li Y, Byers AL, Peltz CB, Barnes DE. Veterans with Agent Orange exposure were nearly twice as likely to be diagnosed with dementia, even after adjusting for the competing risk of death, demographic variables, and medical and psychiatric comorbidities. JAMA Neurol. 2021 Apr 1;78(4):473-477.
Apolipoprotein E ( APOE) ε4 status moderates the relationship between close-range blast exposure and cognitive functioning. Wooten T, Sullivan DR, Logue MW, Fonda JR, Fortier CB, DeGutis J, McGlinchey R, Milberg W, Esterman M. An APOE gene variant may make people more vulnerable to cognitive problems from explosive blasts. J Int Neuropsychol Soc. 2021 Apr;27(4):315-328.
Preclinical validation of a potent γ-secretase modulator for Alzheimer's disease prevention. Ryerson KD et al. A new drug may help prevent Alzheimer's by modulating, rather than inhibiting, a key enzyme involved in forming amyloid plaques. J Exp Med. 2021 Apr 5;218(4):e20202560.
Synapsin-caveolin-1 gene therapy preserves neuronal and synaptic morphology and prevents neurodegeneration in a mouse model of AD. Wang S, et al. SynCav1 gene therapy may be an option for Alzheimer’s disease and potentially in other forms of neurodegeneration of unknown etiology. Mol Ther Methods Clin Dev. 2021 Mar 29;434-450.
Prevalence of central nervous system-active polypharmacy among older adults with dementia in the US. Maust DT, Strominger J, Kim HM, Langa KM, Bynum JPW, Chang CH, Kates HC, Zivin K, Solway E, Marcus C. In 2018, an analysis of 1.2 million older adults with dementia found that 13.9% filled prescriptions consistent with CNS-active polypharmacy, increasing their risk for impaired cognition, fall-related injury, and death. JAMA. 2021 Mar 9;325(10):952-961.
Prediabetes Is associated with brain hypometabolism and cognitive decline in a sex-dependent manner: A longitudinal study of nondemented older adults. Sundermann EE, Thomas KR, Bangen KJ, Weigand AJ, Eppig JS, Edmonds EC, Wong CG, Bondi MW, Delano-Wood L. Prediabetes may affect cognition through altered brain metabolism, and women may be more vulnerable to the negative effects of glucose intolerance. Front Neurol. 2021 Feb 19;12:551975.
Seizures are a druggable mechanistic link between TBI and subsequent tauopathy. Alyenbaawi H, Kanyo R, Locskai LF, Kamali-Jamil R, DuVal MG, Bai Q, Wille H, Burton EA, Alison WT. Post-traumatic seizures are linked to the spread of abnormal Tau following traumatic brain injury and anticonvulsant drugs can lower the level of abnormal Tau proteins in neurons, preventing cell death. Elife. 2021 Feb 2;10;e58744.
Integrating human brain proteomes with genomewide association data implicates new proteins in Alzheimer's disease pathogenesis. Wingo AP, Liu Y, Gerasimov ES, Gockley J, Logsdon BA, Duong DM, Dammer EB, Robins C, Beach TG, Reiman EM, Epstein MP, De Jager PL, Lah JJ, Bennett DA, Seyfried NT, Levey AI, Wingo TS. This study identified 11 genes that are consistent with causing Alzheimer’s disease. Nat Genet. 2021 Feb;53(2):143-146.
Relationship between retinal vascular occlusions and cognitive dementia in a large cross-sectional cohort. Chan AX, Bakhoum CY, Bangen KJ, Bakhoum MF. Individuals with retinal vascular occlusions have a higher prevalence of dementia. However, this association is secondary to shared underlying risk factors in this population, such as older age and stroke. Am J Ophthalmol. 2021 Jan 30:S0002-9394(21)00047-7.
Neurotoxic microglia promote TDP-43 proteinopathy in progranulin deficiency. Zhang J et al. Microglial toxicity contribute to TDP-43 proteinopathy during neurodegeneration. Nature. 2020 Dec;588(7838):459-465.
Association of anticholinergic medications and AD biomarkers with incidence of MCI among cognitively normal older adults. Weigand AJ, Mondi MW, Thomas KR, Campbell NL, Galasko DR, Salmon DP, Sewell D, Brewer JB, Feldman HH, Delano-Wood L; Alzheimer's Disease Neuroimaging Initiative. Anticholinergic medicines, used for a broad array of conditions from allergies to hypertension, may be associated with an increased risk of cognitive decline. Neurology. 2020 Oct 20;95(16): e2295-e2304.
MicroRNA-195 rescues ApoE4-induced cognitive deficits and lysosomal defects in Alzheimer’s disease pathogenesis. Cao J, Huang M, Guo L, Zhu L, Hou J, Zhang L, Pero A, Ng S, El Gaamouch F, Elder G, Sano M, Goate A, Tcw J, Haroutunian V, Zhang B, Cai D. Researchers uncovered a novel regulatory mechanism of the miR-195 protein targeted at cell structure inbalance, cognitive deficits, and Alzheimer’s pathology. Mol Psychiatry. 2020 Jul 6;10.1038/s41380-020-0824-3.
Benefits and harms of prescription drugs and supplements for treatment of clinical Alzheimer-type dementia. Fink HA, Linskens EJ, MacDonald R, Silverman PC, McCarten JR, Talley KMC, Forte ML, Desai PJ, Nelson VA, Miller MA, Hemmy LS, Brasure M, Taylor BC, Ng W, Ouellette JM, Sheets KM, Wilt TJ, Butler M. Cholinesterase inhibitors and memantine slightly reduced short-term cognitive decline and cholinesterase inhibitors slightly reduced reported functional decline, but differences versus placebo were of uncertain clinical importance. Ann Intern Med. 2020 May 19;172(10):656-668.
Brief cognitive tests for distinguishing clinical Alzheimer-type dementia from mild cognitive impairment or normal cognition in older adults with suspected cognitive impairment. Hemmy LS, Linskens EJ, Silverman PC, Miller MA, Talley KMC, Taylor BC, Ouellette JM, Greer NL, Wilt TJ, Butler M, Fink HA. Many brief, single cognitive tests accurately distinguish clinical Alzheimer-type dementia (CATD) from normal cognition in older adults but are less accurate in distinguishing mild CATD from normal cognition or CATD from mild cognitive impairment. Ann Intern Med. 2020 May 19; 172(10):678-687.
Diagnosis and treatment of clinical Alzheimer's-type dementia: a systematic review. Fink HA, Hemmy LS, Linskens EJ, Silverman PC, MacDonald R, McCarten JR, Talley KMC, Desai PJ, Forte ML, Miller MA, Brasure M, Nelson VA, Taylor BC, Ng W, Ouellette JM, Greer NL, Sheets KM, Wilt TJ, Butler M. Biomarkers can be a useful way of testing for Alzheimer's disease. Rockville (MD): Agency for Healthcare Research and Quality (US):2020 Apr. Report No.: 20-EHC003.
Type 2 diabetes interacts with Alzheimer disease risk factors to predict functional decline. Thomas KR, Bangen KJ, Weigand AJ, Edmonds EC, Sundermann E, Wong CG, Eppig J, Werhane ML, Delano-Wood L, Bondi MW; Alzheimer's Disease Neuroimaging Initiative. Patients with both diabetes and Alzheimer's disease risk factors showed greater cognitive decline than those with one or the other. Alzheimer Dis Assoc Disord. 2020 Jan-Mar;34(1):10-17.
NOTCH3 is non-enzymatically fragmented in inherited cerebral small-vessel disease. Young KZ, Lee SJ, Zhang X, Pearl Cartee NM, Torres M, Keep SG, Gabbireddy SR, Fontana JL, Qi L, Wang MM. Small-vessel disorder cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) arises from mutations in the human gene encoding NOTCH3 and results in vascular smooth muscle cell degeneration, stroke, and dementia. The paper links the signature molecular genetic alterations present in individuals with CADASIL to a post-translational protein alteration in degenerating brain arteries. J Biol Chem. 2020 Feb 14;295(7):1960-1972.
Endothelial immune activation by Medin: potential role in cerebrovascular disease and reversal by monosialoganglioside-containing nanoliposomes. Karamanova N, Truran S, Serrano GE, Beach TG, Madine J, Weissig V, Davies HÁ, Veldhuizen J, Nikkhah M, Hansen M, Zhang W, D’Souza K, Franco DA, Migrino RQ. Medin is a candidate novel risk factor for aging-related cerebrovascular disease and vascular dementia. J Am Heart Assoc. 2020 Jan 21;9(2):e014810.
Objective subtle cognitive difficulties predict future amyloid accumulation and neurodegeneration. Thomas KR, Bangen KJ, Weigand AJ, Edmonds EC, Wong CG, Cooper S, Delano-Wood L, Bondi MW; Alzheimer's Disease Neuroimaging Initiative. Patients with subtle cognitive difficulties showed signs of brain changes linked to cognitive decline and Alzheimer's disease. Neurology. 2020 Jan 28;94(4):e397-e406.
Neuromodulation for apathy in Alzheimer's disease: a double-blind, randomized, sham-controlled pilot study. Padala PR, Boozer EM, Lensing SY, Parkes CM, Hunter CR, Dennis RA, Caceda R, Padala KP. Repetitive transcranial magnetic stimulation may be safely used in people with Alzheimer's disease and may improve apathy, function, and some aspects of cognition. J Alzheimers Dis. 2020;77(4):1483-1493.
Activity of the poly(A) binding protein MSUT2 determines susceptibility to pathological tau in the mammalian brain. Wheeler JM et al. Targeting abnormal tau through the suppression of a gene called MSUT2 (the mammalian suppressor of tauopathy 2) shows promise. Sci Transl Med. 2019 Dec 18;11(523):eaao6545.
Aggregate interactome based on protein cross-linking interfaces predicts drug targets to limit aggregation in neurodegenerative diseases. Balasubramaniam M, Ayyadevara S, Ganne A, Kakraba S, Reddy Penthala N, Du X, Crooks PA, Griffin ST, Shmookler Reis RJ. A revelation of the architecture of insoluble-aggregate networks that may reveal targets susceptible to interventions to ameliorate protein-aggregation diseases. iScience. 2019 Oct 25;20:248-264.
Association of early-onset Alzheimer disease with elevated low-density lipoprotein cholesterol levels and rare genetic coding variants of APOB. Wingo TS, Cutler DJ, Wingo AP, Le NA, Rabinovici GD, Miller BL, Lah JJ, Levey AI. Elevated LDL-C levels were associated with a higher probability of having early-onset Alzheimer's disease. JAMA Neurol. 2019 Jul 1;76(7):8-9-817.
Large-scale proteomic analysis of human brain identifies proteins associated with cognitive trajectory in advanced age. Wingo AP, Dammer EB, Breen MS, Logsdon BA, Duong DM, Troncosco JC, Thambisetty M, Beach G, Serrano GE, Reiman EM, Caselli RJ, Lah JJ, Seyfried NT, Levey AI, Wingo TS. Older patients who showed greater cognitive stability had increased levels of proteins involved with mitochondrial activities or synaptic function. Nat Commun. 2019 Apr 8;10(1):1619.
Use of an Alzheimer's disease polygenic risk score to identify mild cognitive impairment in adults in their 50s. Logue MW, Panizzon MS, Elman JA, Gillespie NA, Hatton SN, Gustavson DE, Ondreassen OA, Dale AM, Franz CE, Lyons MJ, Neale MC, Reynolds CA, Tu X, Kremen WS. An Alzheimer's disease polygenic risk score can be used to correctly identify adults with mild cognitive impairment who are only in their 50s. Mol Psychiatry. 2019 Mar;24(3):421-430.
Association of cognitive function with Amyloid-β and tau proteins in the vitreous humor. Wright LM, Stein TD, Jun G, Chung J, McConnell K, Fiorello M, Siegel N, Ness S, Xia W, Turner KL, Subramanian ML. Low levels of amyloid-β and tau proteins, biomarkers of Alzheimer's disease in eye fluid, were significantly associated with low cognitive scores. J Alzheimers Dis. 2019;68(4):1429-1438.

Download PDF
 Could cholesterol medicine reduce dementia risk in seniors?
Could cholesterol medicine reduce dementia risk in seniors?
 VA study reveals dementia risks unique to people with African ancestry
VA study reveals dementia risks unique to people with African ancestry
 Head trauma, PTSD may increase genetic variant's impact on Alzheimer's risk
Head trauma, PTSD may increase genetic variant's impact on Alzheimer's risk