Office of Research & Development |
 |
Diabetes is a chronic disease in which the body cannot produce or properly use insulin. Normally, insulin brings sugar out of the bloodstream and into cells. If the body cannot make insulin or does not respond to it, the sugar stays in the bloodstream. As a result of high blood sugar levels, damage eventually occurs to blood vessels and organs.
More than 30 million Americans have diabetes, according to the Centers for Disease Control and Prevention, and 84 million more Americans are at risk to develop the disease. Many Veterans have the disease, including some who developed it as a result of being exposed to herbicides while serving in Vietnam.
Symptoms of diabetes include blurry vision, excessive thirst, fatigue, frequent urination, hunger, and weight loss. Persons with diabetes need to have their hemoglobin A1c levels checked every three to six months.
A1c is a measure of average blood glucose during the previous two to three months. It is one of the markers, along with blood pressure and cholesterol control, of good diabetes care.
There are three major types of diabetes. Type 1 diabetes is usually diagnosed in childhood. In this type of diabetes, the body makes little or no insulin, so daily injections of insulin are needed.
Type 2 diabetes usually occurs in adults. In this type of diabetes, the pancreas does not make enough insulin to keep blood glucose levels normal, often because the body does not respond well to insulin. Between 90 and 95 percent of adults with diabetes have Type 2 diabetes. More are at risk due to overweight or obesity.
The third type of diabetes is gestational diabetes, high blood glucose that develops during pregnancy in a woman who does not have diabetes.
Diabetes affects nearly 25 percent of VA's patient population. The disease is also the leading cause of blindness, end-stage renal disease, and amputation for VA patients.
Fighting for Veterans, Life & Limb
The VA has been at the forefront of diabetes research since VA researcher Rosalyn Yalow was awarded the Nobel Prize for her groundbreaking insulin-measuring technique, developed in a 1950s Bronx VA janitor's closet. Today, VA researchers across the country are investigating new and innovative approaches to save the lives and limbs of diabetic Veterans.
VA researchers are studying innovative strategies and technologies, including group visits, telemedicine, peer counseling, and internet-based education and case management, to enhance access to diabetes care and to improve outcomes for patients.
In addition, VA researchers are working to develop better ways to prevent or treat diabetes, especially in special populations such as the elderly, amputees, minorities, spinal cord-injured patients, and those with kidney or heart disease.
For more on Diabetes, visit our Cardiovascular Disease topic page.
If you are interested in learning about joining a VA-sponsored clinical trial, visit our research study information page.
Two of VA's three Nobel laureates have done important work to benefit Veterans with diabetes. The late Dr. Rosalyn S. Yalow received the Nobel Prize for Physiology or Medicine in 1977 for her work in developing the radioimmunoassay, an extremely sensitive way to measure insulin and other hormones in the blood. The technique made possible major advances in diabetes research and in diagnosing and treating hormonal problems related to growth, thyroid function, and fertility.
Dr. Andrew V. Schally also received the Nobel Prize in Physiology or Medicine in 1977 for his discovery that the hypothalamus links the nervous system to the endocrine system via the pituitary gland. He is currently doing research, along with teams of national and international researchers, on growth hormone-releasing hormone (GHRH). Among other possibilities opened up by Schally's work with GHRH is the possibility of reducing or eliminating the need for diabetics to regularly inject insulin.
In 2013, an international research team including Schally devised a way to transplant healthy cells into the body without the usual risk of rejection. The study involved a middle-aged man with diabetes, but it may be relevant to a range of other diseases as well. The researchers developed what amounts to an artificial pancreas (the place where the body makes insulin), which the patient tolerated well without taking drugs to suppress the immune system.
A 2015 study by Schally and his team evaluated newly developed GHRH agonists' ability to promote the growth and function of pancreatic islet cells, and found that these new agonists may provide an improved approach to treating diabetes. Artificially produced agonists are substances like naturally occurring stimulatory substances produced in the body and therefore can act to stimulate an action in the body. Islet cells, also called Islets of Langerhans, sense blood sugar levels and release insulin to maintain normal levels.
Dr. Schally is still vigorously pursuing cures for diabetes and other illnesses affecting Veterans and others at his laboratory in the Miami VA Healthcare System. His reflections on his VA career, written in 2018, can be found here.
For seven and a half years, researchers involved in a VA cooperative study (CSP 465) followed nearly 1,800 patients who had type 2 diabetes. They were interested in examining cardiovascular disease in patients with diabetes.
The researchers attempted to determine if intensive glucose control in diabetic patients—using medication and other methods to reduce elevated blood sugar levels to levels that are considered normal in people without diabetes—would reduce heart attacks, strokes, and death from cardiovascular disease.
It had been previously shown that improvements in blood pressure and cholesterol levels can reduce cardiovascular disease in patients with diabetes, but no previous study had shown the beneficial effects of glucose control on cardiovascular disease.
VADT researchers showed that intensive glucose control in older patients (mean age of 60 years, with 52% on insulin therapy) whose type 2 diabetes had previously been poorly controlled had no significant effect on the rates of major cardiovascular events such as coronary artery disease and stroke, compared with those who were using standard glucose control measures.
The research team also found that the two groups of patients had similar death rates, and that both groups had similar levels of complications such as diabetic neuropathy and retinopathy, with the exception that patients who used standard glucose control measures had higher levels of albumin in their urine. (Albumin in the urine is a possible indicator of kidney disease.)
Trial researchers concluded that both very high and very low blood sugar levels can be dangerous, and that big swings between high and low levels are also potentially harmful.
As a follow up to VADT, VA researchers looked at whether the improvements in glucose control made by one of the groups in the trial led to long-term improved consequences. They collected information on the VADT cohort for more than nine years of additional study, using VA's electronic records system.
The team found that, after nearly 10 years of follow-up, patients who had been in the intensive-control group had a lower incidence of cardiovascular events after the trial was over, but their survival rates were no better than those of the other group.
In a 15-year, follow-up study published in 2018, the team concluded that the group of Veterans who had received aggressive lowering of blood sugar levels had a non-significant 12% decline in cardiovascular events when compared with those who had received standard therapy. The two groups of Veterans also showed no differences in death from all causes. A long-term trend of reduced kidney events was found to be insignificant, suggesting that there was no carryover benefit from the earlier period.
Maintaining good glucose control was shown to reduce cardiovascular consequences for patients with diabetes at 10 years, the researchers noted. They suggested that in order to keep that benefit, patients must continue to sustain good blood sugar levels.
There are no plans for additional follow up at this time.
Air pollution contributes significantly to diabetes around the world—Outdoor air pollution, even at levels that are considered safe, can lead to an increased risk of diabetes globally according to a study published in 2018 led by researchers from the VA St. Louis Health Care System and the Washington University School of Medicine in St. Louis. The records of 1.7 million Veterans were analyzed for the study. They were linked to data from the U.S. Environmental Protection Agency’s land-based monitoring systems as well as data from space-borne satellites operated by the National Aeronautics and Space Administration.
The research team looked at particulate matter—airborne microscopic pieces of dust, dirt, smoke, soot, and liquid droplets. Previous studies have found that such particles can enter the lungs and invade the bloodstream, contributing to conditions such as heart disease, stroke, cancer, and kidney disease. In diabetes, the team hypothesized that pollution would reduce insulin production and trigger inflammation, preventing the body from converting blood glucose into the energy the body needs to maintain health.
Overall, the team estimated that pollution contributed to 3.2 million new diabetes cases around the world in 2016, representing about 14% of all new diabetes cases in that year. They also estimated that 8.2 million years of healthy life were lost in that year to pollution-linked diabetes.
Patients with diabetes show early signs of chronic kidney disease (CKD)—Doctors have long known that patients with diabetes are at risk for kidney disease. A 2018 study by researchers with the VA MidSouth Health Care Network and the University of Tennessee Health Science Center shows that patients can be suffering from undiagnosed kidney disease even before they are aware they have diabetes.
The team looked at data on 36,794 Veterans diagnosed with diabetes between 2003 and 2013. They found that 31.6% of those Veterans had evidence of CKD before their diabetes diagnosis, based on two common measures of kidney function.
Veterans with higher age, hemoglobin A1c, blood pressure, and body mass index also had a greater risk of CKD, as did those with cerebrovascular disease, congestive heart failure, or peripheral artery disease. The team also found that Asian Americans and African Americans had higher rates of CKD than whites, and that Veterans living in the Northeast had a lower risk of CKD than those in the Midwest, South, and West.
VA Diabetes Prevention Program (DPP) shows results—VA’s DPP program, begun in 2012, is modeled after a program promoted nationally by the Centers for Disease Control and Prevention. It offers participants the opportunity to lose weight through dietary changes and increased physical activity. VA also offers its own MOVE! program, which targets a broad range of patients who are obese or overweight with obesity related conditions, whereas the DPP specifically targets obese individuals with laboratory evidence of prediabetes. Both programs are supported by VA’s National Center for Health Promotion and Disease Prevention in Durham, North Carolina.
In a study published in 2017 led by researchers at the VA Greater Los Angeles Healthcare System, the team found that DPP results in a much greater loss of weight than MOVE! after six months of presentation (9 pounds to 4.2 pounds). The margin was smaller after 12 months, with DPP participants weighing 7.5 pounds less than when the program began and MOVE! Veterans 4.4 pounds less.
The researchers hypothesized that DPP participants lost more weight than the MOVE! group because they had a greater frequency of exercise with a consistent group of team members.
Gestational diabetes and preeclampsia rates higher in women with posttraumatic stress disorder (PTSD)—Gestational diabetes is a condition in which some women without diabetes develops high blood sugar levels during pregnancy. In 90% of gestational diabetes cases, the condition will resolve after the baby is born, although women with the condition are at an increased risk of developing Type 2 diabetes, as are their children. Preeclampsia is a pregnancy disorder characterized by the onset of high blood pressure and often protein in the urine. It increases the risk of poor outcomes for both the mother and the baby.
A team led by researchers from the VA Palo Alto Health Care System and the Stanford University School of Medicine reported, in 2017, that a diagnosis of PTSD was associated with an increased risk of both gestational diabetes and preeclampsia. This finding is consistent with VA’s current understanding that PTSD disrupts both neuroendocrine (the interactions between the nervous system and the endocrine system) and cardiovascular health.
Statin use—Researchers at the VA North Texas Health Care System and their colleagues examined the health records of tens of thousands of Tricare beneficiaries for a nearly 10-year period. Their study, published in 2015, found that the use of statins to lower cholesterol is associated with a significantly higher risk of new-onset diabetes—even in a very healthy population.
They also found that statin use is associated with a very high risk of diabetes complications in this healthy population, and with a higher risk of obesity. High-intensity statin therapy was associated with greater risks for all outcomes.
When clinically indicated, statin use does provide significant cardiovascular benefits. Patients who are advised to take a statin medication should discuss the risks and benefits with their physician.
Nonadherence to diabetes drugs leads to poor health outcomes—Patients who did not adhere early on to their medication treatment for Type 2 diabetes were more likely to have heart attacks and strokes, according to a 2018 study by researchers from the VA MidSouth Healthcare Network and their colleagues. The research team looked at data for more than 159,000 Veterans over an 11-year period.
Patients who did not take their medication as prescribed were 14% more likely to have a heart attack in the five years after starting treatment, compared with those that took their medication regularly. Those not regularly taking their medication were also 22% more likely to have a stroke. The less compliant patients were to their medication regimen, the higher their chances were of having a heart attack or stroke, and to have died during the period.
Improvements in insulin release wane after treatment stops—A set of clinical trials examining young people and adults with Type 2 diabetes or impaired glucose tolerance found that disease progression in adults slowed during medical treatment but resumed after treatment stopped. Young people receiving the same treatment had markedly poorer outcomes with continued disease progression both during and after the treatment.
The 2019 study, part of the Restoring Insulin Secretion (RISE) Adult and Pediatric Medical Studies, was chaired by a researcher from the VA Puget Sound Health Care System. The team compared the use of different treatments among adults that had the aim of preserving beta cell function, which is the key to the body’s ability to make and release insulin. While adult participants showed improvements in beta cell function and blood glucose control while on the treatments, these improvements did not persist after treatment ended.
The article suggests that current therapies for diabetes are primarily maintenance therapies, and that there is still a need to find therapies that will cure the underlying disease.
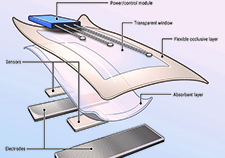
Glucose telemetry system (GTS) developed to monitor hypoglycemia—Up to 30% of hospitalized diabetes patients not treated in intensive care units develop a condition called hypoglycemia, a deficiency of glucose in the bloodstream.
A research team at the Baltimore VA Medical Center has developed a novel glucose monitoring system to help hospitals prevent the development of hypoglycemia in patients. GTS allows the wireless transmission of glucose values from a continuous monitoring device placed at patients’ bedsides to a monitoring device located at nursing stations. This will allow nurses and other health care providers to be notified early about low glucose values and to implement preventive actions to keep patients from developing the condition.
The technology was described in a 2018 article. The team is now conducting a clinical trial examining the effectiveness of the system in hospitalized patients with diabetes who are treated with insulin and are considered to be at a high risk of developing hypoglycemia while they are inpatients.
Million Veteran Program (MVP) provides clue for possible drug targets for diabetes and heart disease—MVP is a national voluntary research program designed to partner with Veterans receiving their care from VA to study how genes affect health. MVP is building one of the world’s largest medical databases by safely collecting and storing blood samples and health information from one million Veteran volunteers.
Using DNA samples from 300,000 MVP participants, researchers from the Palo Alto VA Health Care System, the Corporal Michael J. Crescenz VA Medical Center in Philadelphia, and the Stanford University School of Medicine have singled out a handful of genetic mutations that govern levels of cholesterol in adults, and that may inform the development and use of drugs for diabetes and cardiovascular disease. The results of their study were published in 2018.
Veterans who carried one of three genetic mutations showed improved cholesterol profiles in their blood and a decreased risk of either diabetes, heart disease, or abdominal aortic aneurysms, depending on the gene mutation. Mutations in the ANGPTL4 gene affected the development of diabetes, and the researchers hope a drug can be found or developed that will mimic the beneficial mutation in that gene.
Support from friends and family linked to better diabetes control—Many people with diabetes experience emotional distress from diabetes symptoms, the stress of keeping up with care regimens, and fear of complications from the disease.
Autonomy support is a type of social support that encourages patients to take an active role in their own health care, by respecting their wishes and goals and offering help when needed. According to a 2018 study by the VA Center for Clinical Management Support in Ann Arbor, Michigan, autonomy support from family or friends may help people better control their diabetes by relieving diabetes distress.
By studying 308 Veterans with diabetes, the research team found that high diabetes distress was linked to poor glycemic control. Those with greater autonomy support had greater glycemic control than those without.
GRADE trial—VA researchers are participating in a National Institutes of Health study to compare the long-term benefits and risks of four diabetes drugs in combination with metformin. The study, called the Glycemic Reduction Approaches in Diabetes (GRADE) trial, is expected to include some 5,000 participants nationwide.
Metformin is the first medication doctors typically use when treating Type 2 diabetes. If metformin does not control the disease, doctors may add one of several other drugs, all of which have been shown to lower blood sugar levels in studies. However, no previous long-term study has focused on which drug combination works best and has the least side effects.
The four drugs being studied are sulfonylurea, dipeptidyl peptidase-4 inhibitor, glucagon-like peptide-1 agonist, and long-acting insulin. The estimated primary completion date of the study is 2021.
Lack of durable improvements in β-Cell function following withdrawal of pharmacological interventions in adults with impaired glucose tolerance or recently diagnosed Type 2 Diabetes. RISE Consortium. In adults with impaired glucose tolerance or recently diagnosed Type 2 diabetes, interventions that improved β-cell function during active treatment failed to produce persistent benefits after treatment withdrawal. Diabetes Care. 2019 Sep;42(9):1742-1751.
Vitamin D supplementation and prevention of Type 2 Diabetes. Pittas AG et al. Among persons at high risk for Type 2 diabetes not selected for vitamin D insufficiency, vitamin D3 supplementation did not result in a significantly lower risk of diabetes than placebo. N Engl J Med. 2019 Aug 8;381(6):520-530.
Intensive glucose control in patients with Type 2 Diabetes – 15 year follow-up. Reaven PD, Emanuele NV, Witala WL, Bahn GD, Reda DJ, McCarren M, Duckworth WC, Haward RA; VADT investigators. Participants with Type 2 diabetes who had been randomly assigned to intensive glucose control for 5.6 years had a lower risk of cardiovascular events than those who received standard therapy only during the prolonged period in which the glycated hemoglobin curves were separated. N Engl J Med. 2019 Jun 6:380(23):2215-2224.
Primary care provider type: are there differences in patients’ intermediate diabetes outcomes? Everett CM, Morgan P, Smith VA, Woolson S, Edelman D, Hendrix CC, Berkowitz T, White B, Jackson GL. No clinically meaningful difference in diabetes outcomes exist among patients with different types of primary and supplemental providers. JAAPA. 2019 Jun;32(6):36-42.
Variations in VA and Medicare use among Veterans with diabetes: impacts on ambulatory care sensitive conditions hospitalizations for 2008, 2009, and 2010. Rose DE, Rowneki M, Sambamoorthi U, Fried D, Dwibedi N, Tseng CL, Jani N, Yano EM, Helmer DA. Neither VA nor Medicare may address complex Veterans’ health needs in Veterans with diabetes age 66 or older dually enrolled in VA and Medicare. Med Care. 2019 Jun;57(6):425-436.
Urocortin 2 gene transfer reduces the adverse effects of a Western diet on cardiac function in mice. Kim YC, Giamouridis D, Lai NC, Guo T, Xia B, Fu Z, Gao MH, Hammond HR. Gene transfer of the UCn2 gene may be of potential therapeutic benefit in people with diabetes mellitus at risk of heart failure. Hum Gene Ther. 2019 Jun:30(6)6923-701.
Association of glucose concentrations at hospital discharge with readmissions and mortality: a nationwide cohort study. Spanakis EK, Umpierrez GE, Siddiqui T, Zhan M, Snitker S, Fink JC, Sorkin JD. Veterans with diabetes who had hypoglycemia or near normal glucose values during their last day of hospitalization had higher rates of 30-day readmission and post-discharge mortality. J Clin Endocrinol Metab. 2019 Sep 1;104(9):3679-3691.
Prior antibiotic exposure and risk of type 2 diabetes among Veterans. Davis PJ, Liu M, Alemi F, Jensen A, Avramovic S, Levy E, Hayes RB, Schwartz MD. Any and repeated exposure to certain antibiotics may increase diabetes risk among Veterans. Prim Care Diabetes. 2019 Feb;13(1):49-56.
Metformin intervention prevents cardiac dysfunction in a murine model of adult congenital heart disease. Wilmanns DC, Pandey R, Hon O, Chandran A, Schilling JM, Forte E, Wu Q, Cagnone G, Bais P, Philip V, Coleman D, Kocalis H, Archer SK, Pearson JT, Ramialison M, Heineke J, Patel HH, Rosenthal NA, Furtado MB, Costa MW. Congenital heart disease and obesity can lead to heart failure, but treatment with metformin, a widely used diabetes drug, can prevent the condition. Mol Metab. 2019 Feb;20:102-114.
Older adults and diabetes prevention programs in the Veterans Health Administration. Lee PG, Damschroder LJ, Holleman R, Moin T, Richardson CR. Diabetes prevention programs delivered in person or online can be similarly effective in older and younger Veterans. Diabetes Care. 2018 Dec;41(12)2644-2647.
Results from a trial of an online diabetes prevention program intervention. Moin T, Damschroder LJ, AuYoung M, Maciejewski ML, Havens K, Ertl K, Vasti E, Weinreb JE, Seinle NI, Billington CJ, Hughes M, Makki F, Youles B, Holleman RG, Kim HM, Kinsinger LS, Richardson CR. An intensive, multifaceted online diabetes prevention program had higher participation but similar weight loss compared to an in-person program. Am J Prev Med. 2018 Nov;55(5):583-591.
Differences in health outcomes associated with initial adherence to oral antidiabetes medications among Veterans with uncomplicated Type 2 diabetes: a 5-year survival analysis. Gatwood JD, Chisholm-Burns M, Davis R, Thomas F, Potukuchi P, Hung A, Kovesdy CP. People who are non-adherent to treatment are more likely to experience detrimental health outcomes within the first 5 years of antidiabetes therapy. Diabet Med. 2018 Nov;35(11):1571-1579.
Genetics of blood lipids among ~300,000 multi-ethnic participants of the Million Veteran Program. Klarin D et al. From the DNA of nearly 300,000 Veterans, scientists have singled out a handful of genetic mutations that govern levels of cholesterol and may also inform the development and use of drugs for cardiovascular disease and diabetes. Nat Genet. 2018 Nov;50(11)-1514-1523.
The potential role of fatty acids in treating diabetic neuropathy. Yorek MA. Unsaturated fatty acids have potential for treating diabetic neuropathy. Curr Diab Rep. 2018 Aug 25; 18(10):86.
The 2016 global and national burden of diabetes mellitus attributable to PM2·5 air pollution. Bowe B, Xie Y, Li T, Yan Y, Xian H, Al-Aly Z. The global toll of diabetes attributed to air pollution is significant. Reduction in exposure will yield substantial health benefits. Lancet Planet Health. 2018 Jul:2(7):e301-e312.
Supplemental oxygen improves in vivo mitochondrial oxidative phosphorylation flux in sedentary obese adults with type 2 diabetes. Cree-Green M, Scalzo RL, Harrall K, Newcomer BR, Schauer IE, Huebschmann AG, McMillin S, Brown MS, Orlicky D, Knaub L, Nadeau KJ, McClatchey PM, Bauer TA, Regensteiner JG, Reusch JEB. Targeting muscle oxygenation could improve exercise function in Type 2 diabetes. Diabetes 2018 Jul;67(7):1369-1379.
Diabetes distress and glycemic control: the buffering effect of autonomy support from important family members and friends. Lee AA, Piette JD, Heisler M, Rosland AM. Autonomy support from main health supporters may contribute to better glycemic control by ameliorating the effects of diabetes distress. Diabetes Care, 2018 Jun;41(6):1157-1163.
Individual differences in regulatory mode moderate the effectiveness of a pilot mHealth trial for diabetes management among older Veterans. Dugas M, Crowley K, Gao GG, Xu T, Agarwal R, Kruglanski AW, Steinle N. mHealth technologies can help older adult improve their diabetes management, but a one size fits all approach may yield suboptimal outcomes. PLoS One. 2018 Mar 7;13(3):e)192807.
Evidence of chronic kidney disease in Veterans with incident diabetes mellitus. Gatwood J, Chisholm-Burns M, Davis R, Thomas F, Potokuchi P, Hung A, Kovesdy CP. Evidence of chronic kidney disease is common among Veterans before a diabetes diagnosis, and certain populations throughout the country, such as minorities, may be afflicted at higher rates. PLoS One. 2018 Feb 9; 13(2):e0192712.
Overtreatment and deintensification of diabetic therapy among Medicare beneficiaries. Maciejewski ML, Mi X, Sussman J, Greiner M, Curtis LH, No J, Haffer SC, Kerr EA. Medicare recipients are more frequently overtreated than undertreated for diabetes. Medicare recipients who are overtreated for diabetes rarely have their regimens deintensified. J Gen Intern Med. 2018 Jan;33(1):34-41.
The effect of continuous glucose monitoring in preventing inpatient hypoglycemia in general wards: the glucose telemetry system. Spanakis EK, Levitt DL, Siddiqui T, Singh LG, Pinault L, Sorkin J, Umpierrez GE, Fink JC. The use of CGM values in hospitalized patients can be successfully transmitted to a monitoring device in the nursing station, improving patient surveillance in insulin treated patients with diabetes. J Diabetes Sci Technol. 2018 Jan;12(1):20-25.
Statins for primary prevention in physically active individuals: do the risks outweigh the benefits? Mansi IA, English JL, Morris MJ, Zhang S, Mortensen EM, Haim EA. Among healthy physically active individuals, statin use was associated with double the odds of diabetes and diabetic complications without countervailing cardiovascular benefits. J Sci Med Sport. 2017 Jul;20(7):627-632.
Diabetes prevention program translation in the Veterans Health Administration. Moin T, Damschroder LJ, AuYoung M, Maciejewski ML, Datta SK, Weinreb JE, Steinle NI, Billington C, Hughes M, Makki F, Holleman RG, Kim HM, Jeffreys AS, Kinsinger LS, Burns JA, Richardson CR. VA Diabetes Prevention Program participants had higher participation rates and weight loss at six months, but similar weight, A1c, and health expenditures at 12 months compared to VA’s MOVE! program. Am J Prev Med. 2017 Jul:53(1):70-77.
Post-traumatic stress disorder and antepartum complications: a novel risk factor for gestational diabetes and preeclampsia. Shaw JG, Asch SM, Katon JG, Shaw KA, Kimerling R, Frayne SM, Phibbs CS. There is an association between PTSD and antepartum complications such as gestational diabetes and preeclampsia. Paediatr Perinal Epidemiol. 2017 May(3):185-194.
Agonist of growth hormone-releasing hormone as a potential effector for survival and proliferation of pancreatic islets. Ludwig B, Ziegler CG, Schally AV, Richter C, Steffen A, Jabs N, Funk RH, Brendel MD, Block NL, Ehrhart-Bornstein M, Bornstein SR. Evidence that agonists of GHRH represent a promising pharmacological therapy aimed at promoting islet graft growth and proliferation in diabetic patients. Proc Natl Acad Sci USA. 2010 Jul 13;107(28);12623-8.
Glucose control and vascular complications in veterans with type 2 diabetes. Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, Marks J, Davis SN, Hayward R, Warren SR, Goldman S, McCarren M, Vitek ME, Henderson WG, Huang GD; VADT investigators. Intensive glucose control in patients with poorly controlled Type 2 diabetes had no significant effect on the rates of major cardiovascular events, death, or microvascular complications with the exception of progression of albuminuria. N Engl J Med. 2009 Jan 8;360(2):129-39.
The Veterans Affairs Implantable Insulin Pump Study; effect on cardiovascular risk factors. Duckworth WC, Saudek CD, Giobbie-Hurder A, Henderson WG, Henry RR, Kelley DE, Edelman SV, Zieve FJ, Adler RA, Anderson RJ, Hamilton BP, Donner TW, Kirkman MS, Morgan NA. Implantable insulin pump therapy in insulin-requiring patients with Type 2 diabetes has advantages over multiple-dose insulin therapy in decreasing the requirement for antihypertensive therapy and for decreasing total and free insulin and insulin antibodies. Diabetes Care. 1998 Oct;21(10):1596-602.

Download PDF
 Veteran disability payments led to fewer hospitalizations
Veteran disability payments led to fewer hospitalizations
 Study links statin use with diabetes progression, points to need for further research
Study links statin use with diabetes progression, points to need for further research
 Can statins help 75-and-overs stay healthy? PREVENTABLE trial will provide answers
Can statins help 75-and-overs stay healthy? PREVENTABLE trial will provide answers
 VA researcher develops 'smart bandage' technology for chronic wounds
VA researcher develops 'smart bandage' technology for chronic wounds