Office of Research & Development |
 |

VA Research Currents archive
March 23, 2017
By Mike Richman
VA Research Communications
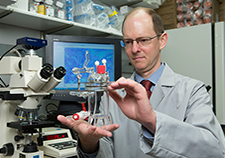
Dr. Jason Wertheim, a surgeon and biomedical engineer at the Jesse Brown VA Medical Center in Chicago, is working on developing an artificial kidney. Here he holds a bioreactor that cultures cells that play a role in creating the artificial organ. (Photo by Jerry Daliege)
Chronic or end-stage kidney failure is a serious health problem in the United States. Some 25 million adults, including many Veterans, have the disease. That means for the rest of their lives they may be on dialysis, the purification of blood as a substitute for a kidney's normal function, or they may receive a kidney transplant—in hopes of avoiding long-term health complications or even death.
Kidney transplantation has a much higher survival rate than dialysis over a five-year period. Despite such success, there aren't enough transplantable kidneys for every person with permanent loss of kidney function who gets cleared for a transplant. An estimated 100,000 patients with the condition, also known as end-stage renal failure, are awaiting a kidney transplant in the U.S. Only about 18,000 such procedures take place each year.
Dr. Jason Wertheim, a surgeon and biomedical engineer at the Jesse Brown VA Medical Center in Chicago, sees many patients with permanent loss of kidney function. With an eye on the dearth of kidneys that are available for transplantation, he's researching ways to compensate for the loss of that organ. Among other projects, he's leading a bioengineering effort to develop tissue for a replacement kidney and thus circumvent the problem of organ shortage.

The kidneys clean blood by removing excess fluid, minerals, and wastes to make urine. (©iStock/HYWARDS)
The kidney, a critical organ, cleans blood by removing excess fluid, minerals, and wastes to make urine. Its inability to properly filter blood can cause a buildup of wastes, the hallmark of chronic kidney disease. Diabetes and high blood pressure are the top causes of kidney disease.
"Transplantation has been very successful in being able to give patients a new lease on life," Wertheim says. "And because organ transplantation is both life-saving and life-improving, patients that have end-stage disease need and want a transplant in many cases. But the quality of cadaveric organs that we get can change over time just based on demographics. Obesity is prevalent in our society, and that leads to livers that might have too much fat content in them. Hypertension can cause progressive kidney dysfunction. So not every organ offered for transplantation is usable. That's why we have more patients that need replacement organs and tissues than the number of donor tissues that are available. There's hope that one day in the future we can develop those tissues for patients who need it."
"The whole issue is to develop something that will actually function the way a kidney would function."
Wertheim is immersed in that effort. His bioengineering project calls for developing three-dimensional scaffolds that originate from animals to support nephron segments, the basic structural and functional units of the kidney, as templates for new cells. After their natural cells are removed, the scaffolds are repopulated with immature kidney cells. The hope is that they will multiply and grow into many adult kidney cell types.
The scaffolds, which contain proteins that give organs their structure, are "replicative of the natural environment of the kidney," Wertheim says. The scaffolds are intended to support the growth of tissue that will eventually become a new kidney.
The project is part of (Re)Building a Kidney (RBK), a consortium led by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) at the National Institutes of Health. The consortium, which includes about 25 biologists and engineers from around the country, is trying to develop tools that will facilitate development of an artificial kidney in the future. Its goals are to create and implement feasible strategies for engineering replacement kidney tissue, and to devise ways to stimulate regeneration of nephrons in their natural position to restore failing kidney function.
Dr. Deborah Hoshizaki, program director of NIDDK's Division of Kidney, Urologic, and Hematologic Diseases, is director of the consortium, a five-year program that began in 2015.
"We're delighted to have Jason," she says. "He's meticulous, he's doing the right experiments, and he's a wonderful team player. There's added value not only for the consortium to have Jason on board—I think the consortium provides him with added value in terms of direct access to a lot of the expertise that will help move his project forward.

"There just aren't enough kidneys for transplant," she adds. "If we could get everyone to donate kidneys upon their death, that would help out a lot. But in the meantime, can we get a substitute for a donor kidney, and can we bioengineer the kidney? That's where Jason's work is coming together."
Wertheim, who also works on cell-based projects on liver and muscle regeneration and blood vessel development, has been involved in his kidney endeavor for five years. He's the consortium's only researcher with VA affiliation. He does his lab work at the Jesse Brown VA and at nearby Northwestern University, where he's a transplant surgeon and an assistant professor of surgery.
His project uses an extracellular matrix, a collection of fibrous material that holds cells together within tissues and organs. The matrix contains signals that drive cell differentiation, the process by which a cell becomes specialized in order to perform a specific function. The system serves as a model for nephron development within a full-scale kidney scaffold and sets the stage for further cell differentiation in a perfusion bioreactor, which cultures cells much longer than traditional laboratory-based cell culture. The ability to develop extracellular scaffolds and to add back donor cells to the matrix allows researchers to analyze growth and maturation of the cells in three dimensions.
Here's the challenge: At least 20 different cell types make up a kidney. They would all need to be part of an engineered kidney that replicates the organ's natural functions. Knowing exactly where the cells must be within the engineered organ is tricky. Solving that equation is critical to someday taking a discarded human kidney and growing a replacement kidney with new cells.
"At this stage in the technology," Wertheim says, "we're first looking at how cells respond to the extracellular matrix, what the cells become, and how changes to the matrix can influence how they function."
Wertheim and his team have been experimenting with small animal models, mainly rodents. They remove the kidney from the animals and extract its native cells, leaving only the three-dimensional matrix that gives the kidney its structure, before repopulating the matrix with new cells. "Then through the vasculature [blood vessels in the organ], we can permeate the scaffold to spread the nutrients that support cell growth," Wertheim says. "The cells will grow within the three-dimensional scaffold."
Wertheim says focusing on small animal models has been beneficial "because we can observe how cells grow and interact with the matrix on a smaller scale." He and his colleagues have used some pig kidneys and are in the process of "scaling up" to experiment with larger animals more consistently. They've built many extracellular scaffolds, he says.
Hoshizaki: "The value of the approach that Jason's using is basically being able to take kidneys, in a sense discarded kidneys, being able to strip out the cells, but still using the matrix that's left behind. He's then trying to rebuild a kidney with all of the right cell types to be able to basically start developing, in a sense, a kidney on the shelf."
Wertheim and Hoshizaki say it's premature to predict how long it will take to create an implantable and functional human kidney once the consortium wraps up. At the end of the five-year life of the consortium, according to Hoshizaki, "we'll have a much better idea of which strategies we should invest our money in in terms of creating a new kidney, but right now no one in the consortium knows what will work."
The consortium is trying to be critical in that regard and is "casting a broad net unlike a lot of other efforts," she says. "We don't know what's going to be the best strategy from a research standpoint that would provide us with more information to develop something that can be commercialized."
"Maybe it's going to be a pig kidney scaffold, and re-populating that with human cells," she speculates. "We have people who are using 3D printing to make portions of a kidney. Maybe it will be a hybrid with various elements of the consortium's projects. The whole issue is to develop something that will actually function the way a kidney would function. It would be doing things like concentration, which means something that could reabsorb water, and something that could have the correct ion exchange, so you have the appropriate molecules staying in the urine or being reabsorbed to the kidney and being recycled."
Wertheim isn't the first researcher in the scientific community who has used a naturally made scaffold for the purposes of building a tool to grow a replacement kidney. Still, his work is "innovative and unique," Hoshizaki says.
"He's at the forefront of folks who are doing this," she says. "And I think it's fair to say that he's a leader in carrying out this approach, in taking the kidney from a small animal, stripping it of its cells, and using that as the scaffold for creating a new kidney."
She admires Wertheim's pragmatic approach.
"His project is one of the few [that are] taking a very systematic, perhaps not flashy, view of how we can start to populate these matrices," she says. "And I would say that that's one approach the consortium is interested in being able to advance the science. We are interested in the much more bioengineered type approach, which is one of several approaches we think could be valuable."
She adds: "He recognizes, for example, that depending on how you strip the scaffold, you may be losing what I call all the bells and whistles that tell the cells where they should be, what they should be producing. So you basically have none of the roadmap that's necessary for cells to figure out what they should be doing."
Wertheim is one of several researchers in the consortium who is working on developing scaffolds. The others are silk-based scaffolds, he says.
"We need to look at all different types of scaffolding materials," he says, "because the goal of the consortium, which is quite wide, is to try to tackle the problem from different angles. But really the out-of-the-box thinking is that maybe we could combine some of our natural materials with the synthetic structures that our collaborators are developing to make a hybrid approach. That shows synergy and collaboration within the group, and that's something that's going to be important as the field moves forward."
Hoshizaki welcomes that type of teamwork. She also likes that Wertheim stays in regular contact with members of the consortium who are developing ways to produce large quantities of cells.
"That is part of what we really, really encourage with the group," she says. "That's what defines the consortium, besides the science. You get all these top-notch scientists and A-type personalities together, and they all want to be alpha dog [leader of the group]. We want them all to play well together."
While plugging away on the research front, Wertheim remains passionate about saving lives. He hopes that someday there will be enough tissue-engineered replacement organs for patients.
"Among our patients that have end-stage disease, there's a desperate need for new organs to first sustain their lives and then to enhance their quality of life," he says. "Liver transplantation is a life-saving procedure, and a patient is faced with death when a liver cannot recover on its own. Kidney transplantation is life-saving over the long term, compared with dialysis.
"But as physicians we cannot necessarily perform a transplant immediately when a patient needs it," he adds. "We're dependent upon the supply of altruistic, cadaveric donors, and sometimes patients have to wait a couple of days, weeks, months, and even years. Some patients don't have that amount of time."