Office of Research & Development |
 |
Office of Research & Development |
 |


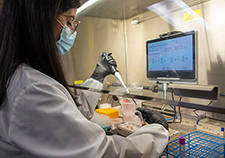
VA researchers probed the reasons why nurses and other health care workers sometimes deviate from established protocols regarding the use of respiratory protective equipment. (Photo: ©iStock/Samara Heisz)
March 2, 2020
Steve Tokar
VHA Communications
"One of our biggest takeaways is that teams should have explicit conversations—such as in team huddles—that address their concerns."
As fears of a coronavirus pandemic persist, it's more critical than ever for nurses and other hospital and clinic staff to use best practices to help keep infections from spreading.
A recent VA study provides insight on why health care workers sometimes fail to use respiratory protective equipment (RPE)—namely, respirator masks— to protect them from getting and spreading airborne infections, and why they sometimes use the equipment when it’s not required. One way the new coronavirus and other dangerous respiratory infections spread is by people coughing or sneezing.

AI to Maximize Treatment for Veterans with Head and Neck Cancer

VA researcher works to improve antibiotic prescribing for Veterans
VA’s Million Veteran Program played crucial role in nation’s response to COVID-19 pandemic
VA Further Develops Its Central Biorepository: VA SHIELD
The VA researchers found that policies and social norms within hospitals tend to reinforce correct RPE use. They also found that this culture of safety can be undermined when health care workers are unsure of risk levels or if they mistrust hospital protocols and rely on their own judgment.
“One of our biggest takeaways is that teams should have explicit conversations—such as in team huddles—that address their concerns,” says Dr. Gemmae Fix, lead author on the research, which appeared in October 2019 in the American Journal of Infection Control.
Fix is a medical anthropologist and health services researcher with Boston University and VA’s Center for Healthcare Organization and Implementation Research (CHOIR), based at the VA medical centers in Boston and nearby Bedford.
Her group conducted 12 focus groups with nurses and nursing assistants at four VA and academic medical centers in the Northeast and Midwest.
The study focused on N-95 respirators, special masks that are individually fitted to cover the nose and mouth and filter out 95% of airborne germs—even tiny droplets. Simpler face masks, also called surgical or medical masks, seen widely in the public since the coronavirus outbreak, block only larger droplets and are not nearly as effective.
Fix’s team found that health care workers generally knew when hospital policy called for using RPE, and that following hospital RPE protocol was seen as “part of the job.” Social norms in the hospitals reinforced this culture of safety. This can be seen in instances like health care workers urging other staff members to don a mask, or organizing respiratory safety training for other hospital workers, such as food service staff, when they observed that RPE protocol was not followed.
Fix notes that N-95 respirators can be uncomfortable, especially when worn for hours at a time, and that previous studies have focused on this as the main driver of poor adherence to protocol. But she says her team found that “while RPE was reported to be uncomfortable, people wanted to follow RPE protocol. RPE misuse was instead driven by ‘personal’ protocols, such as when people did not trust the protocol and instead relied on their experience.”
For example, a patient who is coughing heavily might lead some nurses to put on a respirator mask. But that symptom in itself is not necessarily an indicator for RPE.
The researchers emphasize that when staff follow their own personal safety protocols, this can undermine the broader safety culture. Overuse of RPE, they say, can potentially desensitize hospital staff to the value of correct RPE use and needlessly alarm others. Overuse may also result in RPE being unavailable when it is actually needed.
“Some health care workers worry the protocols inadequately protect them,” says Fix, “so they want to follow their own ‘personal’ protocol and proactively wear RPE even when it is not specified. Mistrusting the safety protocols in place may lead to overuse of RPE, which undermines both the general safety culture and also risks depleting supplies.”
Fix notes the overuse is generally well-intended. “The nurses want to protect themselves and their other patients.”
Fix’s team found that workers in urban hospitals tended to see themselves at higher risk for infection than their rural colleagues because their facilities had many high-risk patients. This led some urban health care workers to perceive that their hospitals did not have enough RPE or that it was not readily accessible when needed. In contrast, rural hospital staff reported RPE as plentiful and accessible.
Emergency departments (EDs) had their own issues. The focus groups suggested a “distinctly different clinical context” at play in these hospital units, says Fix.
“Unlike the other units, patients come into the ED without a working diagnosis,” she explains. “Thus there is the persistent potential that patients may have an airborne infection. Health care workers in the ED likely get acclimated to not having a diagnosis [for the patient] and subsequently not wearing RPE. Not wearing RPE then persists as these health care workers from the ED move through the facility, even after the patient has been given a diagnosis that now requires RPE.”
The authors conclude that because “a large-scale pandemic is always possible,” adherence to RPE protocol may become critical with little advance notice. They recommend that each hospital assess its own unique context and safety culture with regard to RPE use, especially in urban areas or EDs where risk perceptions may differ.
Fortunately, they note, their data provide insight into reasons why health care workers do not follow RPE protocol—and those reasons are usually modifiable.
“RPE use is informed by not only national and local policies, but the local culture,” notes Fix. “Human behavior is complex, but modifiable. Explicit work to address poor adherence, such as team huddles, can help health care workers talk about their concerns, address potential mistrust of the protocols, and ensure everyone is working as part of a culture of safety.”
For information from VA about Novel Coronavirus Disease (COVID-19), as well as links to the latest updates from the Centers for Disease Control and Prevention, visit www.publichealth.va.gov/n-coronavirus/index.asp.
VA Research Currents archives || Sign up for VA Research updates