Office of Research & Development |
 |
Office of Research & Development |
 |


VA Research has awarded $40 million in funding to study the effectiveness of esketamine for treatment resistant depression. (Photo for illustrative purposes only. ©Getty Images/Jay Yuno)
April 12, 2023
"This study is the first to evaluate the comparative effectiveness and cost-effectiveness of esketamine compared to aripiprazole."
Contributed by the VA Connecticut Healthcare System
The Department of Veterans Affairs (VA) has awarded $40 million in research funding to study the effectiveness of esketamine for Veterans and others with treatment resistant depression (TRD).
The VA Aripiprazole vs. Esketamine for Treatment Resistant Depression (VAST-D II) is a multisite study that will compare the effectiveness of two medications used to enhance the effect of standard antidepressants—esketamine (Spravato) and aripiprazole.

VA Researcher Named One of U.S.’ Top Female Scientists

Million Veteran Program director speaks at international forum
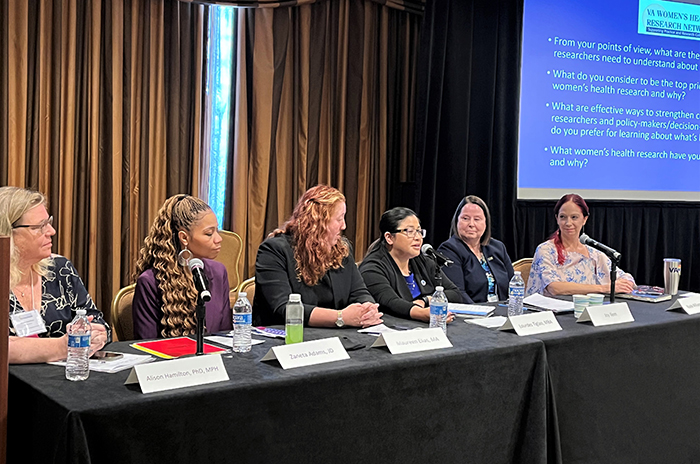
2023 VA Women's Health Research Conference
Patients with TRD, a form of depression that has not responded to multiple previous treatments, are at highest risk to become chronically ill, develop a substance abuse disorder, attempt suicide, or any combination of the three.
“Esketamine represents the only currently FDA-approved approach that holds the promise of being a breakthrough,” said Dr. Somaia Mohamed, associate director of VA’s Northeast Program Evaluation Center (NEPEC), associate professor of psychiatry at Yale University, and principal co-chair of the study. “If it produces greater remission rates, has more sustained benefits with fewer side effects, and lower health-related costs, the benefit to thousands of Veterans and millions of other patients would be substantial.”
The study is the first to evaluate the comparative effectiveness and cost effectiveness of esketamine as compared to aripiprazole, according to Mohamed. The researchers suggest that participants who receive an intranasal dose of esketamine to enhance the effect of standard antidepressants will be significantly more likely to achieve remission for their depression after six weeks of treatment, than those adding aripiprazole.
In 2019, the U.S. Food and Drug Administration (FDA) reviewed intranasal esketamine as a new therapy treatment that can lead to a rapid reduction in symptoms of TRD. The safety and efficacy of esketamine was evaluated in a series of phase III studies that ultimately led to its approval by the FDA for treatment in adults, but did not compare it with other effective strategies.
The newly funded study will be a randomized clinical trial in which more than 900 Veterans across 25 VA sites will receive either intranasal esketamine or oral aripiprazole for up to six months of treatment. This study will assess the efficacy, safety, and acceptability of esketamine in direct comparison to aripiprazole for TRD therapy.
Depressive symptoms will be assessed by using the Quick Inventory of Depressive Symptomatology clinician rating tool, which is a well-validated tool that is easily translated across other depression inventory scales.
In a previous multisite VA study, Mohamed and her colleagues showed the addition of aripiprazole resulted in a significantly greater likelihood of depression remission, compared to switching to bupropion. Later analyses demonstrated that the benefit of using adjunctive aripiprazole among 12-week remitters was sustained for up to six additional months of therapy and was evident whether patients had co-occurring PTSD or not. This was the first study to show one strategy of TRD treatment had some advantage over another, but the gains were small in magnitude and left room for improvement.
“If esketamine produces greater remission rates, the results of this research may provide an empirical basis for revising current practice guidelines for TRD,” Mohamed said. “With this large, multisite study, VA’s role as a leader in improving the treatment for depression would be firmly established.”
Co-chairs for the study are Dr. Michael Thase, from the Corporal Michael J. Crescenz VA Medical Center in Philadelphia, and Dr. James Murrough, from the James J. Peters VA Medical Center in the Bronx, New York.
VA Research Currents archives || Sign up for VA Research updates