Office of Research & Development |
 |
Office of Research & Development |
 |

When growth hormone is low, patients can experience symptoms ranging from fatigue and mood disorders to weight gain and dry skin. (Photo: ©Stock/Shidlovski)
June 12, 2018
By Mike Richman
VA Research Communications
Based on a clinical trial led by a VA investigator, the U.S. Food and Drug Administration has approved an oral drug that is considered a fast, simple, convenient way to determine if a patient has adult growth hormone deficiency (AGHD). The condition is a potential consequence of traumatic brain injury.
The approval of Macrilen (macimorelin) was based on a phase 3 clinical study of Macrilen led by Dr. Jose Garcia, an investigator in the Geriatric Research, Education, and Clinical Center at the VA Puget Sound Health Care System in Seattle. He is also an associate professor at the University of Washington.
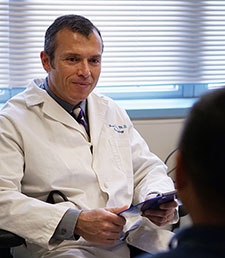
Dr. Jose Garcia is an investigator in the Geriatric Research, Education, and Clinical Center at the VA Puget Sound Health Care System. (Photo by Christopher Pacheco)
The study results appeared online May 31 in The Journal of Clinical Endocrinology & Metabolism. The study was funded by the drug’s maker, Aeterna Zentaris, and included authors from the company, working with an international team led by Garcia.
In the study, the team found Macrilen stimulated the release of growth hormones with comparable accuracy to the insulin tolerance test (ITT), which has long been the standard way of diagnosing AGHD.
Measurement of growth hormone levels is critical to learning if someone has AGHD.
“I’m very excited that the FDA approved macimorelin,” says Garcia, also a member of the Seattle Institute for Biomedical and Clinical Research. “To participate in research that leads to a drug being on the market is the ultimate goal of every researcher. I’m proud of the fact that VA played a key role in this and that our Veterans had a chance to participate in the research.”
He adds: “The availability of this test will make AGHD diagnosis easier and will lead to more patients being tested and eventually treated for AGHD. I anticipate that Macrilen will become the first choice for AGHD diagnosis in most patients given its ease of use, reliability and safety.”
Strongbridge Biopharma, which acquired the U.S. and Canadian rights to Macrilen from Aeterna Zentaris, plans to commercially launch Macrilen later in 2018. AGHD affects about 60,000 adults in the United States and Canada, according to Strongbridge.
"To participate in research that leads to a drug being on the market is the ultimate goal of every researcher."
“In the absence of an FDA-approved oral diagnostic test for AGHD, Macrilen fills an important gap and addresses a medical need for a convenient test that will better serve patients and health providers,” Aeterna Zentaris said after the drug was approved in December 2017.
Macrilen stimulates the release of growth hormones from the pituitary gland—which is important for controlling growth and development—into the circulatory system. After fasting for at least eight hours, a patient takes a liquid form of Macrilen in a small amount based on body weight. Growth hormone levels are then measured in blood samples for about an hour to determine if someone has AGHD.
Direct supervision by a doctor isn’t required.
In contrast, the insulin tolerance test may be challenging in some settings because it calls for a physician to monitor the procedure and for resources that may not be available to every doctor. Those resources include direct supervision from a trained endocrinologist, one nurse, one technician, a room for up to three hours, and direct access to a lab that analyzes glucose levels. The ITT can also be unpleasant for the patient, with several blood draws over the course of at least two hours.
Plus, the ITT should not be used in patients with heart disease or a history of seizures because it causes hypoglycemia, or low blood sugar, in order to produce an accurate result. A patient’s blood sugar must drop below 40 (milligrams per deciliter) for the test to be interpreted, says Garcia.
Many people are uncomfortable with their blood sugar below that mark, Garcia says. He notes that the blood sugar level in about 20 percent of patients won’t go below 40.
“Some patients get really hungry or irritable due to hypoglycemia,” Garcia says. “It’s been reported that others have had seizures or strokes. The ITT is seldom used due to its potentially serious side effects and the fact that it’s cumbersome and costly. It’s the best test but is still risky to perform.”
The Macrilen test does not induce hypoglycemia and is well-tolerated, he says. The most common side effects of the drug are mild and transient. They include dizziness, headaches, fatigue, nausea, hunger, diarrhea, upper respiratory tract infection, hot flashes, excessive sweating, a sore nose and throat, a decline in heart rate, and an altered sense of taste.
Despite the potential and convenience of Macrilen, Garcia explains that the insulin tolerance test, although it’s “impractical and physicians are afraid of using it,” will remain the “gold standard” for diagnosing AGHD.
“Technically, it gets into the fact that we don’t really have another way to say for sure that someone is growth hormone deficient or not,” he says. “It remains the gold standard because that’s what was developed first, and that’s what everything compares to.
“What we can say is that Macrilen performs well compared with the ITT,” he adds. “Macrilen probably is more potent in stimulating growth hormone secretion, if you ask me. But we cannot claim that it’s more accurate based on the design of the [phase 3 trial] and the data we generated.”
More than a decade ago, the Arginine-GHRH (growth hormone releasing hormone) test was the best alternative for diagnosing AGHD. But the drug Geref, the commercial name for a form of GHRH, was voluntarily withdrawn from the U.S. market in 2008. Other currently available tests, such as arginine, clonidine, levodopa, and arginine combined with levodopa, are much less accurate in detecting AGHD.
The glucagon stimulation test, a relatively simple and safe procedure that measures growth hormone levels after injection of a hormone called glucagon, has also been used to diagnose AGHD. But the test lacks accuracy particularly for overweight and obese people, Garcia says. “Until now, patients were often being diagnosed with it anyway for lack of a better alternative.”
“It’s been about a decade since Geref was taken off the market,” he says. “There have been a lot of cases in which the diagnosis was missed. Patients were just not being diagnosed.”
Growth hormone deficiency (GHD) can occur at any age, in both adults and children. The main cause of adult GHD is believed to be hypothalamic or pituitary lesions, which are growths on the pituitary gland. Patients with the condition may experience fatigue, depression, mood disorders, weight gain, reduced lean body mass, high cholesterol, less muscle strength and exercise capacity, thin and dry skin, and impaired mental well-being. AGHD is also believed to be linked to premature death.
Studies of traumatic brain injury (TBI) have found evidence of chronic hypopituitarism. That’s deficient hormone production by the pituitary glands, including growth hormone deficiency.
One of the most cited VA studies on the link between blast-related TBI and AGHD looked at Veterans from the wars in Iraq and Afghanistan with a history of mild TBI, or concussion. Eleven of the 26 Veterans (42 percent) showed abnormal hormone levels indicative of post-traumatic hypopituitarism.
The Department of Defense and the Defense and Veterans Brain Injury Center estimate that 22 percent of combat casualties from Iraq and Afghanistan involve brain injuries. That compares with 12 percent of Vietnam combat casualties.
However, it’s unclear in the medical community whether growth hormone replacement treatment would be effective for mild TBI.
“It has been known for years that AGHD can be a consequence of TBI,” Garcia says. “However, most of the data comes from the pre-9-11 era. We do not know for sure how often it happens in these Veterans. My hope is that the Macrilen test will facilitate the diagnosis of AGHD in our Veterans with TBI.”
In Garcia’s phase 3 study, 140 patients took part in both the Macrilen test and the ITT. The VA hospitals in Seattle and Houston served as research sites.
The researchers found that Macrilen stimulates the pituitary gland with accuracy comparable to that of the ITT to diagnose growth hormone deficiency. Only 1 out of 153 Macrilen tests had to be repeated to meet the threshold for AGHD, compared with 28 out of 157 insulin tolerance tests.
In addition, Macrilen stimulated growth hormone release more powerfully than the ITT. Peak growth hormone levels following use of Macrilen were equal to or higher than those observed during the ITT in about 80 percent of all cases.
Furthermore, Macrilen showed 87 percent sensitivity, the ability of a test to correctly identify people with the disease, and 96 percent specificity, the ability of a test to correctly identify those without the disease.
Garcia anticipates using Macrilen in more clinical studies involving the diagnosis of AGHD. He’s also exploring use of the drug to treat muscle atrophy, in which muscles deteriorate, for example, due to a lack of physical activity.
“It’s possible that this drug or drugs in this family could have other applications,” he says. “Just to give you an example, the FDA recently approved a drug in this family for treating anorexia in dogs. But all other applications for Macrilen or anything in that class are still in the research phase.”
Lance Caver has no problem displaying a tough-guy look: goatee, tattoos, rock-solid face, squinty eyes, neatly cropped hair.
The 46-year-old Army Veteran has parlayed that image into an acting career, landing main roles as a biker, thug, detective, bartender, and soldier in movies with small to large budgets. He’s now in two recently released films, the science fiction movie “Forbidden Power” and the horror movie “Beloved Beast.” He’s playing a school principal in “They Reach,” another horror film that is in production.
He’s also waiting to hear about potential roles in movies in Australia and Scotland.
“This is something I had never even considered in the past,” he says. “It just kind of happened by having my two daughters enrolled in acting classes. I was asked if I could fill a role in a feature movie since I had a look they needed for it, and they would put my girls in it if I did. It’s kind of grown from there.”
Caver may be adept at assuming film roles, but he can’t escape the reality of two difficult health conditions he’s coping with: traumatic brain injury (TBI) and adult growth hormone deficiency (AGHD).
Serving in Iraq from 2003 to 2006, Caver spent time in an Army unit that put him in precarious situations. He says he got “hit hard” many times, including when a rocket-propelled grenade slammed into his Humvee.
He’s since experienced bad migraine headaches, as well as persistent neck and back pain. “I’ve just learned to live with it,” says Caver, who is on permanent disability.
Traumatic brain injuries can lead to AGHD. Caver got an AGHD diagnosis when he took part in the phase 3 clinical trial of the drug Macrilen led by Dr. Jose Garcia of the VA Puget Sound Health Care System (see main article).
His AGHD symptoms include fatigue and weight gain. He’s on human growth hormone medication and has reported feeling better overall, with increased energy levels and improvements in sleep and feelings of depression.
In the trial, Garcia and his team found Macrilen to be comparable to the more traditional insulin tolerance test (ITT) in diagnosing AGHD. Given that Macrilen was still in the experimental stage at the time, Caver was diagnosed with AGHD purely based on the ITT. The Macrilen results from the 140 patients in the study were measured blindly.
Caver preferred the Macrilen test by far.
“Oh my God, the [ITT] just made me feel horrid,” he says. “I can’t even explain the feeling I had when I went through that test. The Macrilen test was a piece of cake. Man, that was a world of difference. I didn’t have the horrific feelings I had with the other one. I still had to lay there for a while and go through the whole testing process. The Macrilen left a bad taste in my mouth, but I’d take that rather than suffer from the feelings I had with the other one.”
Caver, who is 5-feet-7, weighed no more than 180 pounds in Iraq. But he ballooned up to 240 after his honorable discharge from the service in 2008.
Through healthy eating and regular exercise, mostly on the treadmill, he’s reduced his weight to 215. But he’s had trouble losing any more.
“I still can’t lose weight by eating right and exercising, even though I try to work out to what my headaches can tolerate,” he says. “I just cannot get it off. My biggest thing now is figuring out how to drop the weight. I’d love to lose about 50 more pounds. I’m sure that will help with everything.”
Caver says doctors have explained to him that his inability to lose weight may, in part, be due to having abnormal hormone levels in the pituitary gland, a small body attached to the base of the brain that is important for controlling growth and development.
“From what I’ve been told, adult growth hormone deficiency usually leads to fat accumulation and growth hormone replacement in adult patients,” he says. “Growth hormone replacement in adults with growth hormone deficiency results in a reduction of fat mass and abdominal fat mass, in particular.”
AGHD isn’t directly linked to headaches. However, both may occur as a result of TBI.
“I’d never had headaches before, especially like these, until Iraq,” Caver says. “These headaches have since gotten worse and have never gone away.”
Meanwhile, Caver continues battling his ailments so he can perform on the set. He says he sometimes struggles to remember lines when he’s presented with a lengthy dialogue. But he’s worked at times with other Vets with TBI in the acting business, noting that “most have been very patient and understanding” about the challenges he faces.
“You just have to ignore the fact that there are lots of cameras, crew, and other equipment around you while doing it,” he says. “Some scenes have been very hard for me to do, like letting someone point a [mock] weapon at me and then shoot it, considering how much combat I’ve been in. For my own piece of mind, I have to inspect every weapon on the set to ensure it’s a prop. I still cringe every time I have to act out those scenes, though.”
--- Mike Richman
VA Research Currents archives || Sign up for VA Research updates