Office of Research & Development |
 |
Office of Research & Development |
 |


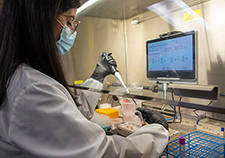
Dr. Jason Dazely, an infectious disease specialist at the Southern Nevada VA, checks in on Dr. Parisa Khan as she prepares to donate her plasma. (Photo courtesy of Southern Nevada VA)
June 2, 2020
Mike Richman
VA Research Communications
"I want to be a message of hope and gratitude for our Veterans."
Dr. Parisa Khan is a clinical pharmacist who specializes in infectious diseases at the VA Southern Nevada Healthcare System. As a recovered COVID-19 patient, she’s a candidate to help others who are experiencing symptoms from the disease.
Recently, Khan donated her convalescent plasma at the Southern Nevada VA. People who have recovered from the disease have immune-boosting antibodies in their plasma—convalescent plasma—that are being used as an experimental treatment for critically ill COVID-19 patients.
The U.S. Food and Drug Administration (FDA) has regulated COVID-19 convalescent plasma as an investigational COVID-19 treatment. It’s a way to treat critically ill patients who have few options left.
Khan followed the news about convalescent plasma antibody treatments during her 41-day quarantine, when she was mostly asymptomatic. She was eager to be a donor.

VA center training the next generation of researchers in blood clots and inflammation

AI to Maximize Treatment for Veterans with Head and Neck Cancer

VA researcher works to improve antibiotic prescribing for Veterans
VA’s Million Veteran Program played crucial role in nation’s response to COVID-19 pandemic
“I’m more than happy to do this,” she said while donating her plasma at a blood bank in Las Vegas. “I consider myself so fortunate to be able to recover from the disease. The best news possible is that my experience can hopefully help other people.
“I want to be a message of hope and gratitude for our Veterans,” she added. “If my plasma can help Veterans who are coming to our hospital, that would be great. I want more employees who have recovered and can come back to work to take something from this story and think about donating themselves.”
Khan’s donation was part of VA’s most far-reaching effort thus far to study potential treatments for COVID-19. The agency is cooperating with the Mayo Clinic, a renowned U.S.-based medical center, on an expanded access study to evaluate convalescent plasma therapy for COVID-19. The FDA has approved an expanded access protocol for convalescent plasma transfusions. Expanded access is a way for a patient with a life-threatening or otherwise serious condition to gain access to an investigational medical product for treatment outside of a clinical trial when no comparable or satisfactory therapies are available.
As of May 20, more than 80 VA medical centers had signed up for the program so their patients could benefit from convalescent plasma transfusions. More than 180 units of convalescent plasma had been transfused to 158 Veterans fighting the disease. Typically, only one unit is given to a Veteran, but patients can receive a maximum of two.
Convalescent plasma is the liquid part of blood that contains antibodies. The body generates these blood proteins to fight against specific infections, such as COVID-19. The plasma must be typed as if someone were giving a transfusion of blood with red or white cells in it. Plasma by itself doesn’t contain red or white cells.
Antibodies can directly attack the virus that causes COVID-19, as well as cells that the virus has entered. Thus, it’s believed that COVID-19 patients may improve faster if they receive plasma from those who have recovered from the disease.
Plasma transfusions are generally safe and well-tolerated by most patients. But side effects have been reported, including mild fever, allergic and transfusion reactions, acute lung injury, and bronchospasm, a sudden constriction of the muscles in the walls of the bronchioles. There is also a rare risk of infectious disease transmission from donated plasma.
VA’s Office of Research and Development (ORD) played a key role in enabling VA medical centers to participate in the Mayo Clinic program. ORD developed an infrastructure to support any VA facility, including those without research programs, that wants to take part. VA clinicians at those facilities can request access to the investigational convalescent plasma treatment for their patients. The VA medical centers are working under the Mayo Clinic’s protocol for convalescent plasma.
The plasma is being collected at American Association of Blood Bank (AABB) locations. VA is not collecting the plasma.
It is unknown how many Veterans will donate plasma or how many will require convalescent plasma, according to Dr. Molly Klote, a senior official in ORD.
In addition to the Mayo Clinic program, VA researchers are developing or joining clinical trials that will offer even more treatment opportunities for Veterans with COVID-19. Many trials are in the planning stage, and some have already enrolled volunteer participants.
The trials demonstrate the ability of VA—America’s largest integrated health care network, with a significant capacity for research—to work with government and industry partners on a wide range of solutions during the COVID-19 national health crisis.
“We’re in a position to do things that no one else in the world can do to improve the health of our Veterans, the nation, and the world,” VA Secretary Robert Wilkie said. “VA is bringing all of its expertise to bear during this crisis, and now we’re leading the way on research into pharmaceuticals and treatments that could improve the lives of thousands of patients.”
VA Research Currents archives || Sign up for VA Research updates