Office of Research & Development |
 |

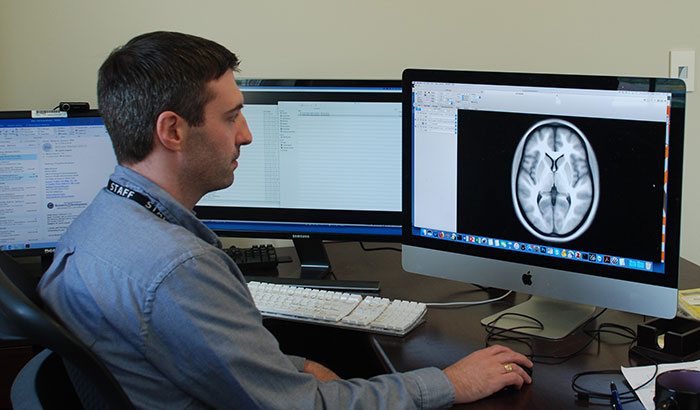
Dr. Evan Gordon is with the Center of Excellence for Research on Returning War Veterans at the Central Texas Veterans Healthcare System. (Photo by Lisa Boynton)
July 19, 2018
By Mike Richman
VA Research Communications
"We're trying to associate symptoms and outcomes with specific [brain] regions that are not talking to each other as well as they should."
Current methods of diagnosing a traumatic brain injury are limited in their ability to show doctors how the brain is working.
Cognitive tests and standard magnetic resonance imaging (MRI) scans are likely to indicate which areas of the brain are damaged. But gaining a deeper, more detailed look into how the brain is functioning remains a challenge.
Dr. Evan Gordon and Dr. Steven Nelson, cognitive neuroscientists in the Center of Excellence for Research on Returning War Veterans at the Central Texas Veterans Healthcare System, are working to meet that challenge. They are experimenting with a form of magnetic resonance imaging called functional MRI (fMRI), a common research tool that is not yet used clinically. It can show how a traumatic brain injury (TBI) may derail communication between areas of the brain that are normally in sync.
The doctors hope those details will make it easier to rehabilitate a brain region that isn’t functioning properly. They believe one possible therapeutic approach could be transcranial magnetic stimulation (TMS), which uses a magnetic field that the brain translates into electrical activity.
VA researchers are experimenting with various brain stimulation technologies to treat TBI and PTSD. But the U.S. Food and Drug Administration has not yet approved any of those technologies for this purpose.

Million Veteran Program director speaks at international forum
2023 VA Women's Health Research Conference

Self-harm is underrecognized in Gulf War Veterans
“The way that doctors diagnose the severity of TBI now is very simplistic,” Gordon says. “They ask, `Were you unconscious? How long were you unconscious?’ But if you have a precise map of a person’s brain organization, you have a much better idea of what brain areas you may want to stimulate with a TMS machine. This precise characterization of brain function would allow us to give much better diagnostic or potentially prognostic information to that patient. We would hope to see even mild brain injuries by getting good estimates of brain network communication. But all of this is in the future: things we are thinking about, things we are starting to work on.”
Gordon and Nelson believe fMRI could also prove useful for patients with PTSD, although they’re taking a somewhat different approach than with TBI. In cases of PTSD, they have a better idea of the brain circuits that are not functional, with the focus on the connection between the front of the brain and a mid-brain region called the amygdala.
“With PTSD, we’re trying to map these circuits very precisely [in each patient] so we can figure out exactly where they are on the surface of the cortex,” says Gordon, referring to the largest region in the brain. “That’s because their location varies slightly from one person to another. Once we know exactly where they are, we can try to target them using TMS.”
Although fMRI doesn’t yet have strong clinical applications, Gordon thinks the medical community should look into using it more, namely as a diagnostic tool. That’s because “for many sorts of disorders and injuries, structural MRIs have not helped doctors figure out what’s going on in the brain and what to do,” he says, noting that a reliable technology doesn’t exist to diagnose a TBI.
The fMRI procedure, through an advanced scanner, measures brain activity by detecting changes in blood flow in the brain. It creates images or maps of brain functioning; increased blood flow to the activated areas of the brain shows up on fMRI scans. A structural MRI provides a map of the brain’s structure but doesn’t detect blood flow or other metabolic processes. A brain injury could thus go undetected.
“If you have a tumor in your brain, a structural MRI can tell you that,” Gordon says. “A structural MRI can also tell you if you’ve suffered a penetrating brain injury or a stroke. It can give you decent information about what parts of the brain are damaged, and we have an idea about what parts of the brain do what. But structural MRI has not been diagnostically useful for TBI, PTSD, depression, or schizophrenia. For the disorders where something is happening to the brain, but it’s not so terrible that there’s a visible structural injury, you need to look at how the brain is functioning differently than it should be. We want to go in that direction.”
Traumatic brain injury is the signature wound from the wars in Iraq and Afghanistan. The Department of Defense and the Defense and Veterans Brain Injury Center estimate that 22 percent of combat casualties from Iraq and Afghanistan involve brain injuries. That compares with 12 percent of Vietnam combat casualties.
Symptoms of TBI include headaches, irritability, sleep disorders, memory problems, slower thinking, and depression.
Many Veterans have also been diagnosed with PTSD, which can trigger symptoms similar to those of TBI. They include anger, guilt, depression, sleep problems, and re-living trauma through flashbacks and nightmares.
There’s more to the ambitions of Gordon and Nelson, who are pioneering a data-driven approach. One of their main goals has been to figure out—in the case of a TBI—how much data are needed to determine which brain regions are not communicating properly. The more time a patient spends in the fMRI scanner, the richer the data on his or her brain function. Taking this approach, the researchers believe, will give them a chance to locate subtle changes in the brain that produce TBI symptoms.
In regard to the high-data approach, Gordon says, “We’re probably the first medical team that’s doing this major push with any kind of neurological or neuropsychiatric disorder, certainly TBI and PTSD.”
He and his team have determined that for the measurements they’re using, collecting an hour to an hour and a half of data is as good as amassing five hours of data. “That leads us toward being more practical for clinical approaches,” he says. “It turns out that to get good accurate measurements using neuroimaging, you need to collect a lot more data and average that data within a single person to get a good understanding of that person’s brain organization.”
He adds: “This is potentially expensive and arduous. It’s going to depend on how beneficial it ultimately is for diagnosis, prognosis, and treatment recommendations. It’s also going to depend on what the alternatives are.”
In the past, researchers typically collected only about five minutes of fMRI data. But increasing awareness of how inaccurate those measurements can be has prompted an increase to about 20 minutes, Gordon notes. “That's becoming more common for data that are going to be averaged across a group,” he says. “But in our case, it’s clear that you need more than that for individual-focused research.”
While in the fMRI scanner, the patient is in a resting state. That means he or she is asked to lie still and let the mind wander. Even when a person isn’t doing anything, there’s a “baseline level” of communication between regions in the brain, Gordon says. The patient is allowed to exit the scanner every 15 minutes or whenever he or she needs a break.
“If you show the patient pictures or stimuli or ask them to think about things, then you’ll see brain activation and time-locked activity,” he says. “The MRI signals go up in response to the patient doing things. However, if you ask them to be in a resting state, you see a bunch of different regions in the brain that seem to spontaneously fluctuate in their activity. You can start looking for associations between the activity time courses in different regions.”
The rich data the researchers hope to collect could yield more insight into how specific brain regions work together.
“So maybe I have a region in the middle front of the brain,” Gordon explains. “Activity there goes up and stays up, and then goes down and up and down and down. At the same time, I’m looking at a region in the middle back of the brain. Its activity will mirror the first region. The level of activity will be highly correlated in those two regions. The only way to understand that is to think that these regions must be communicating with each other. That suggests they are strongly connected.”
Once the scientists have an idea which regions are connected, Gordon says, they can look at how strong those connections are.
“With traumatic brain injury, what we’re seeing, for instance, is very widespread degradation in the ability of these brain regions to have a networked communication,” he says. “They don’t seem to be talking to each other nearly as well. We‘re starting to get very precise estimates of that disconnect, as well as how much degradation there’s been. We’re trying to figure out if the degradation in these two regions is predictive of this person having more problems with emotional control or having disrupted social lives or having memory loss—things like that. We’re trying to associate symptoms and outcomes with specific regions that are not talking to each other as well as they should.”
Thus far, Gordon has led two studies that have made use of fMRI through a 3 Tesla scanner at the Center of Excellence for Research on Returning War Veterans. That scanner has twice the power of scanners found in local hospitals, he says.
One of the studies appeared in the journal Neuron in August 2017. It involved 10 non-Veterans who were showing symptoms of TBI and PTSD. The participants received a structural MRI, a task-related fMRI, and a resting-state fMRI.
The other study, which appeared in the Journal of Neurotrauma in March 2018, included 26 Veterans with TBI and PTSD. Each took part in 3.5 hours of resting-state fMRI and diffusion tensor imaging, a form of structural MRI that looks at how water spreads through the brain. In many people with TBIs, water spreads in the middle of the white matter in the brain, indicating white matter damage.
Both studies reached some similar conclusions.
“We saw that in both studies, with the fMRI in particular, you had to collect a lot of data to get reliable measures,” Gordon says. “Once you collected a lot of data, your measures were very reliable, very robust. We got very precise measures on each person of the functional connectivity, the degree to which brain areas are talking to each other efficiently. One of the things we showed in the Journal of Neurotrauma paper is if we didn’t get those measures, we could not see relationships between TBI and the fMRI and PTSD symptoms. We were able to see those only by collecting a lot of data on each person and by getting highly reliable measures.”
“One of the overall messages is that you have to collect a lot of data to get very precise brain maps of a person,” he adds.
Combining fMRI scans with a large data collection in cases of TBI is at least five years from human application, according to Gordon.
For now, Gordon and his colleagues want to expand their experimental work to a larger sample of about 100 Veterans. To better associate symptoms and outcomes with brain regions that aren’t communicating with each other as well as they should, the researchers want to “figure out if there are behaviorally relevant subgroups inside the larger TBI group and then compare the data,” Gordon says. Subgroups are groups of people who may have similar injuries and are experiencing similar symptoms.
A subgroup the scientists believe will emerge is one that has suffered TBI-related damage to circuits that regulate emotion and is experiencing increased PTSD symptoms.
Gordon thinks the data will be more reliable than before because the Center of Excellence for Research on Returning War Veterans has obtained a new 3 Tesla MRI scanner that can produce much higher-resolution images than the one used previously.
“A doctor wants to know what sort of sensitivity and specificity of diagnosis you can get,” he says. “For example, one group with a particular neural deficit may be more susceptible to PTSD. Another group with a different deficit might have more problems with memory. A third group may have experienced a similar impact and has been knocked unconscious for a similar time. But it has few behavioral and neural deficits and thus might not have `TBI,’ despite having suffered a classic TBI event. This subtyping idea in traumatic brain injury is the next big place we’re going.”
VA Research Currents archives || Sign up for VA Research updates