Office of Research & Development |
 |


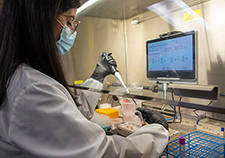
The Human Engineering Research Laboratories (HERL) has been helping meet the demand for VA medical supplies triggered by the COVID-19 crisis, making such items as face shields, desk shields, and nasal testing swabs. (Photo courtesy of the Human Engineering Research Laboratories)
July 8, 2020
Mike Richman
VA Research Communications
In recent months, the coronavirus and the disease it causes, COVID-19, have touched nearly every industry in the United States. Many government agencies and private businesses have pivoted—whether by mandate or voluntarily—from how they ordinarily do things. That has included changing their production models to help meet the demand for medical supplies triggered by the health crisis.

Cleaned, sterilized, and bagged testing swabs ready for use in the VA health care system. (Photo by Bill George)
The Human Engineering Research Laboratories (HERL) has made that transition, too. HERL, a large VA facility that does research, development, and testing on an assortment of technologies, has been producing nasal testing swabs, face shields, and desk shields, and has worked with the VA NY Harbor Healthcare System in Brooklyn to develop an enclosure-like structure on wheels that can be rolled from one hospital bed to another to protect health care workers caring for patients.
Parents and grandparents of HERL staff have contributed by sewing cloth face coverings. Dr. Garrett Grindle, the assistant director of engineering at HERL, has been leading the design and fabrication of other devices.
The items are intended for use by staff and Veterans at VA medical centers. Some of the face shields have been donated to HERL’s academic affiliate, the University of Pittsburgh.
HERL, a collaborative effort between the VA Pittsburgh Healthcare System and the University of Pittsburgh, has a strong team of engineers and perhaps the best fabrication and standards testing facilities in VA. HERL's projects include wheelchair technologies, advanced prostheses, robots, and other innovative systems that improve the quality of life for people with disabilities, such as lost limbs and spinal injuries. The facility is home to the VA Center for Wheelchairs and Robotics Engineering and is based in a state-of-the-art research and development park that includes government, academic, and private industry innovators.
"I am extremely proud of the team at HERL. They have risen to the challenge of assisting with VA's response to COVID-19 and have performed outstandingly."
HERL’s director, Dr. Rory Cooper, says the center has been investing about 30% of its engineering work hours into developing products that are related to the pandemic. The production of these items has been compatible with the facility’s existing equipment.
“The transition has largely been seamless not only because of our infrastructure, but also because we have very smart people,” Cooper says. “It doesn’t do you any good to have all the equipment if you don’t have people not only that know how to run it but are also adept enough to change direction.”

VA center training the next generation of researchers in blood clots and inflammation

AI to Maximize Treatment for Veterans with Head and Neck Cancer

VA researcher works to improve antibiotic prescribing for Veterans
VA’s Million Veteran Program played crucial role in nation’s response to COVID-19 pandemic
HERL started making COVID-19 items in early April at the request of Dr. Ali Sonel, chief of staff at the Pittsburgh VA. As of mid-June, the technology center had produced about 250 face masks, 50 face shields, 10,000 testing swabs, and five desk shields, plus a prototype of the bedside device.
The swabs, which are printed on HERL’s laser-powered 3D printing machine, have been made for use at the Pittsburgh VA and the Philadelphia VA Medical Center. But Cooper says HERL may ramp up its production that would call for producing as many as 100,000 per week, should VA hospitals around the country need them.
Thus far, HERL has been making nasopharyngeal swabs that are inserted in the nostril and extend behind the eye. A health care professional helps conduct the test. The HERL team has been working with two men at the Pittsburgh VA—Dr. Patrick Strollo, a pulmonologist, and Robert Swiatkowski, an expert in sterile processing—to ensure the safety and effectiveness of the swabs. If HERL increases its output of the swabs, Cooper imagines the facility will produce different types, depending on VA’s needs. Recently, VA officials asked HERL to develop a snare nasal swab, which is more convenient than the nasopharyngeal swab because a health care specialist is not needed to help collect the sample.
With the possible large-scale production of snare swabs, “VA could potentially build the capability for many people who enter a VA medical facility to do a screening test, including patients, doctors, nurses, and therapists, if there were a need or plans to do so,” Cooper explains. “People could potentially take a quick test, which includes answering a few questions, get a temperature measurement, and provide a rapid sample with a snare swab if warranted. The results could determine the pathway of the person going into the facility.”
Making the swabs is much more complicated than it appears. “They have to be strong enough to not crack or break when you insert them up a person’s nose,” Cooper says. “But they’ve got to be flexible enough to get up the nose for a sample and not cause pain. You’ve got to scoop up enough gunk in order to test for the virus. They also must be cleaned and sterilized and tracked. Once used, they must be properly contained so they’re not contaminated and so viruses don’t deteriorate on the way to the lab. Ultimately, the challenge with a snare swab is to make a comfortable yet effective snare.”
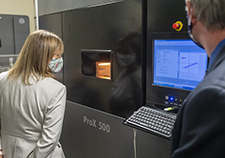
VA Acting Deputy Secretary Pamela Powers peers through the view port to watch the fabrication of COVID-19 testing swabs. HERL may ramp up its production to as many as 100,000 swabs per week. (Photo by Bill George)
HERL’s machine shop features a wide variety of manual and computer-controlled machines capable of cutting and shaping metal, plastic, and other materials. For the desk shields, the face shields, and the bed shield, HERL is using its computer numerical control (CNC) router table, its CNC laser cutter, and a host of other machines.
Most of the face shields have been provided to VA research scientists, driver training instructors, and wheelchair seating clinic therapists. A driving training instructor could be working with a Veteran who is seeking a license to operate an adaptive vehicle, or with a Veteran who must complete a driver’s training program because of a disabling condition. The desk shields are meant, for example, to protect people in a cubicle from others who work in that space, or a receptionist in an office or the lobby of a building who greets visitors and answers their questions.

HERL director Dr. Rory Cooper wears one of the cloth face coverings that his facility has helped produce. (Photo courtesy of the Human Engineering Research Laboratories)
“When you come to a VA hospital, a person is typically there who answers questions on where you need to go,” Cooper says. “That person normally is at a desk. But if you’re standing, and that person is sitting without a shield, then you may be too close.”
A portable, aerosol-protective device for use next to hospital beds is the most complex item that HERL has designed and fabricated during the pandemic. It was created by Sam Fares, an engineer at the Brooklyn Campus of the VA NY Harbor Healthcare System. HERL collaborated with Fares to build the device, which shields clinicians from the coronavirus and other infectious diseases while they tend to patients. The plexiglass frame gets positioned at the head of the bed and a protective sheet blocks airborne droplets from the patient. The device contains arm holes for clinicians and access ports for ventilator hoses and other medical equipment used during intubation and other procedures. Staff can easily roll the protective device from one bed to another.
Cooper comments on the various requirements the team had to satisfy for the device: “You’ve got to be able to have both the doctor and nurse work together. You also have to adjust the height of the device to accommodate a short or tall doctor. You’ve got to be able to make it compatible with existing VA hospital beds in rooms so it can be moved from place to place. Then you’ve got to be able to clean it and sterilize it, so once the patient gets better and goes home you don’t contaminate anyone else.”
It’s possible, Cooper says, that HERL will produce several of the devices for VA hospitals, depending on the extent of the COVID-19 impact on Veterans.
VA’s Technology Transfer Program has filed a patent application to protect the invention. The program works to commercialize VA inventions to benefit Veterans and the American public.
This isn’t the first time HERL has redirected its efforts to solve an urgent user problem . Two years ago, VA issued a patient safety alert based on reports from VA facilities of burns to Veterans or fires involving home oxygen delivery systems. The problem stemmed from the blowback valve that’s in place to prevent a fire caused by an electrical short in the oxygen concentrator from going into a Veteran’s nose or lungs. Some users who changed out the hoses would forget to put the blowback valve back in place.
To solve the problem, the VA Prosthetics and Sensory Aids Service reached out to HERL, which designed a device that prevented a person from removing the blowback valve without using specific tools. HERL’s invention led to a patent filing that is now under review in the VA Technology Transfer Program.
VA’s Technology Transfer Assistance Project (TTAP) supported the design and development of the device. TTAP is a partnership between the Technology Transfer Program and HERL to develop prototypes that bridge the gap to the commercialization of products meant to help Veterans.
Cooper believes HERL will continue responding to the coronavirus pandemic as long as VA needs its help. That may be until a vaccine has been clinically tested and is approved by the Food and Drug Administration, he notes.
“I am extremely proud of the team at HERL,” he says. “They have risen to the challenge of assisting with VA’s response to COVID-19 and have performed outstandingly. The work of the team at HERL has likely helped slow the spread of the disease and has assisted VA health care providers in saving the lives of Veterans.”
HERL is just one of several VA entities that are redirecting its talents and ingenuity to help during the coronavirus pandemic.
The Advanced Platform Technology Center (APT Center), known for developing innovative technologies that serve Veterans with limb loss and sensory, motor, or cognitive deficits, is producing items that offer protection from the virus.
APT engineers, based at the Louis Stokes VA Medical Center in Cleveland, are creating a reusable antiviral facemask that is intended to kill pathogens on contact. Conventional polymer-based masks only trap bacteria and viruses. A separate APT team has designed and prototyped a facemask and pump system to filter out potential virus-carrying aerosol mist from the exhaled air of patients using nebulizers. The goal is to reduce the exposure of first responders and other medical personnel to the coronavirus and medication during nebulizer treatment.
Plus, the APT Center’s technical innovation specialist, Frank Zitko, is combining his engineering know-how with the clinical insights of Dr. Matthew Kellems, an anesthesiologist, and Robert Bearss, a nurse anesthetist, to develop a new version of an intubation box. During intubation, a tube is inserted into a patient’s body to provide oxygen. Clinicians can be exposed to infectious respiratory droplets and aerosols that patients emit. The goal of the device is to shield clinicians from coronavirus and other infectious diseases. The box contains arm holes and access ports for medical equipment that is often used during intubation. The device has some similarities to the bedside device from the Brooklyn VA and HERL described above, but each has its unique features.
At two other VA medical centers, the Minneapolis VA and the Puget Sound VA in Washington State, researchers are also making protective equipment and other supplies that support VA’s response to the pandemic. The researchers are collaborating with the VA Innovation Ecosystem, the U.S. Food and Drug Administration, the U.S. National Institutes of Health (NIH), and America Makes, which specializes in technology research, discovery, creation, and innovation in additive manufacturing and 3D printing. The equipment includes:
Clinical evaluations of 3D-printed device designs are available on the NIH 3D print exchange COVID-19 response web site.
--- Mike Richman
VA Research Currents archives || Sign up for VA Research updates