Office of Research & Development |
 |


Dr. William Marchand’s most recent study on sailing as a recreational therapy included 25 Veterans, each of whom had had at least one mental health condition or substance use disorder.
July 9, 2021
By Mike Richman
VA Research Communications
Dr. William Marchand is an avid recreational sailor. To him, the scenery, wind, and water are calming and compatible with mindfulness.
Mindfulness involves focusing on the present moment, while calmly acknowledging and accepting one's feelings, thoughts, and bodily sensations. Walking, hiking, meditation, and yoga can help someone achieve a state of mindfulness—as can any other type of sport or recreational activity—if one is focused on the present.
So an idea dawned on Marchand, a psychiatrist at the VA Salt Lake City Health Care System. Understanding that many Veterans with mental conditions and substance use disorders do not experience full remission from conventional treatments or engage in such therapies at all, he and VA colleagues embarked on testing a recreational program that would encourage participation by offering an enjoyable experience, while imparting a therapeutic benefit.
His choice: mindfulness-based therapeutic sailing (MBTS).
"There isn’t a rule that says treatment can’t be fun."
“There isn’t a rule that says treatment can’t be fun,” he reasons.
Marchand has led three pilot studies thus far, including one with nature exposure through recreational sailing and another with nature exposure through sailing combined with mindfulness training. The latter teaches one to have a non-judgmental awareness of the present and to differentiate that from autopilot thinking, or thinking instinctively, about the past and the future, according to Marchand.
“The practice involves being aware of that autopilot thinking and bringing one back to the present moment,” he says. “That’s primarily what we wanted as the take home message about mindfulness, something that people could grasp in a short period of time and could start using.”
Marchand’s most recent research was based on what he and his colleagues learned from the first two pilot studies: The concept appeared to be feasible and warranted further evaluation, and the sessions should include only sailing and not classroom-only sessions. The study included mindfulness training and was aimed at establishing a version of MBTS that would be ready for a rigorous controlled study with a large number of participants. The findings appeared in the journal Military Medicine in February 2021.

VA Researcher Named One of U.S.’ Top Female Scientists

Million Veteran Program director speaks at international forum
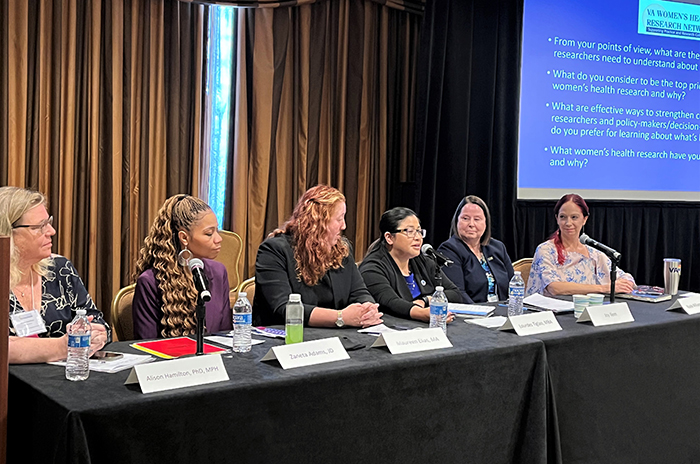
2023 VA Women's Health Research Conference
The study included 25 Veterans, all but two of whom were men (see sidebar). Each participant had at least one mental health condition or substance use disorder, and more than 90% had two or more conditions. With help from the Park City Sailing Association in Utah, the Veterans engaged in three sailing sessions of at least an hour each at the Jordanelle Reservoir State Park in Utah.
The researchers used a physical activity enjoyment scale to determine how much the participants liked the program. Scores indicated that most of the participants enjoyed the sailing, and that it was potentially linked to a decline in substance use treatment services. But the latter finding, Marchand cautions, is a correlation and not a cause and effect. He says it’s unclear how MBTS is related to less need for substance abuse treatment.
“The sailing possibly helped participants decrease substance use, and thus less treatment was needed,” Marchand says. “But more rigorous studies will be needed to further explore this finding.”
The results must be considered preliminary, according to Marchand and his team.
“However, these findings corroborate results from a previous pilot study and indicate that MBTS holds promise as a complementary [program] that could result in enhanced treatment engagement and-or outcomes for the population studied,” the researchers write. “A randomized controlled trial of MBTS is warranted. Further, the model of a three-session [program] combining mindfulness training with nature exposure could be adapted for other types of nature exposure, such as hiking, snowshoeing, or other complementary [therapies], including equine-assisted activities and therapies.”
Marchand is confident that MBTS can improve treatment engagement or response among Veterans in conventional programs, similar to the potential of other complementary therapies, such as yoga, tai chi, or meditation. However, he would not recommend MBTS as a stand-alone treatment for a mental health condition because of its limited evidence base. A conventional treatment, such as medication or one of the trauma-focused psychotherapies VA uses to treat patients with PTSD—cognitive processing therapy or prolonged exposure—must be used first or in parallel with a complementary therapy, such as MBTS, he notes.
“Over time and with lots of research, many things once considered complementary develop as stand-along treatments,” he says. “But recreational sailing would most likely remain a complementary intervention long-term.”
Based on the post-sailing questionnaire, researchers in Marchand’s most recent study also concluded that MBTS is linked to increases in psychological flexibility and mindfulness. Psychological flexibility, he says, is the ability to respond to situations in a manner that helps the person and is also consistent with his or her personal values.
“One way of thinking about it is the level of rigidity in one’s thinking versus the ability to be adaptive and perhaps most importantly to be able to engage in flexible behaviors,” he says. “A good example is that when we are upset, we tend to respond in an emotional way. So a Veteran has an argument with his or her spouse and feels upset and angry and tends to respond the way they’ve always responded in habitual behavior patterns that often aren’t very helpful. With psychological flexibility, one can better take stock and say, `Hmmm, this is what I always do, but it doesn’t work very well. Maybe I need to try something different.’”
The researchers didn’t measure PTSD-specific outcomes, for example, by using a PTSD symptom scale. “Increases in mindfulness and psychological flexibility would be expected to be beneficial for PTSD, but that must be explored in future studies,” he says.
One goal of developing the MBTS program was to increase treatment participation. Marchand was surprised by the level of engagement, with 96% of the participants attending all of the sessions. That was an “excellent result” that strongly supports the use of MBTS from an engagement in treatment standpoint, he says. “This was primarily a proof of concept study, and our ability to assess outcomes was limited due to the small sample size. That said, outcome data were promising, but clearly more rigorous studies are needed with much larger sample sizes,” he says.
Participation was up, he says, mainly because all of the sessions in the study included sailing.
All of this begs the following questions: How practical is MBTS as a long-term therapy for Veterans experiencing mental and substance abuse disorders? And how many Veterans can VA help with this type of therapy?
“That is difficult to answer until we do more rigorous studies that can assess cost benefit data to determine if [MBTS] would be cost-effective to implement at other VA facilities,” Marchand says. “Also, the motivation and ability to implement a program like this will vary from one VA site to another. So even if MBTS is shown to be beneficial and cost-effective in larger studies, it is impossible to know how widely it will be disseminated.
“However, that said, MBTS is a model that could be implemented with community partners–like we did with the Park City Sailing Association in Utah– in many parts of the country at least during the summer months,” he adds. “Using this model at our site, we could likely serve around 100 Veterans per summer season.”
But not all VA medical centers are close to a body of water.
“That’s one of the major limitations,” Marchand says. “Part of our work has been to develop the general concept of a therapy involving recreation and nature exposure and not necessarily tie it to sailing. For example, hiking is much more accessible and also is a nature exposure. So it might be that this model could be adapted to other more accessible forms of nature exposure.”
Marchand says there are various ways he could carry out a randomized controlled trial on the effectiveness of a recreational therapy. One approach would be to focus on a specific population, such as Veterans with PTSD, and randomize the participants into a treatment group that includes a recreational therapy and mindfulness training, and a control group with standard treatment. He explains that controls are challenging for studies like this because it’s impossible to blind participants and the study team. The number of Veterans would likely be around 120, with 60 in each group.
“The concept is really combining a mindfulness program with something else that is healing like nature exposure and using it to engage Veterans,” he says, “because one of the real problems we have is engaging Veterans in treatment. So combining treatment with something that is often perceived as pleasurable tends to be more engaging than inviting someone to sit in a therapy office for six to eight sessions.”
Currently, Marchand’s main research focus is on equine services, or interaction with horses, and equine-assisted psychotherapy. In one of his upcoming studies, the treatment group will include equine services with no mindfulness training, and the control group will include standard treatment.
“We’ve become interested in taking this general concept and applying it to other activities, such as hiking, which is probably just as accessible and might be just as effective, and equine services,” he says. “We want to use the outcome measures from our pilot studies, as well as diagnosis specific measures, such as PTSD symptom scales. I’m not sure that we’ll necessarily continue to explore the sailing piece. Everything is speculative at this point.”

Kristine Bean, an Army Veteran diagnosed with PTSD and depression, has been able to gain control of her thoughts through mindfulness training. “You focus on the moment you’re in,” she says.
It’s the noise that Army Veteran Kristine Bean remembers the most: The constant sounds of rockets, mortars, tracers, and nighttime firefighting that filled the skies during her deployment from early 2003 to mid-2004 at Camp Slayer, a U.S. base near the international airport in Iraq’s capital, Baghdad. The blasts rang in her head for extended periods.
“It was all kinds of bullets flying all night,” she recalls.
Bean has since been diagnosed with PTSD and depression. She maintains weekly contact with a therapist at VA Salt Lake City and has taken part in cognitive processing therapy, one of the main trauma-focused psychotherapies VA uses to treat patients with PTSD.
Two years ago, Bean participated in a complementary therapy. She signed up for a study that focused on mindfulness training and sailing for Veterans with PTSD, substance use disorder, and other mental health conditions (see main story). Dr. William Marchand of VA Salt Lake City led the study, which involved three one-hour classes of mindfulness training, followed by one-hour sailing sessions on Deer Creek Reservoir at Jordanelle Reservoir State Park in Utah. As she saw it, the sailing was a way to practice the mindfulness training, which involved periods of meditation.
Bean found the mindfulness training to be very helpful.
“It seemed like a training of being in the present, recognizing your thoughts wandering, and refocusing them on what you want, instead of what just happened to come to mind,” she says. “It seemed more a matter of being able to train yourself to recognize thought patterns that you didn’t want to dwell on and refocus on what you’re doing in the present. You focus on the moment you’re in. We also practiced breathing techniques.”
When asked if she’s applied what she learned through the mindfulness training, Bean says “100% yes.”
“It felt like someone had given me a tool to use when I have anxiety issues, so it’s been good,” she says. “Unfortunately, I noticed that some people didn’t seem to understand. I felt like they were sitting there not trying to think of anything to clear their mind. They didn’t understand that you want to use [mindfulness] during times of stress or feeling out of control. You can redirect your focus and gain control of your thoughts. I would say the people who were directed there through the court system for substance abuse seemed not to quite understand it as well. I don’t know why. But it seemed like the majority of people were enjoying the mindfulness training and the sailing.”
Bean spoke to VA Research Currents several days before the customary Fourth of July fireworks celebration. She said she probably wouldn’t attend the fireworks for fear of flashbacks to her experiences in Iraq, but that she wouldn’t hide from them, either. She’s gone to Canada in the past to avoid the Independence Day festivities because “the fireworks were too much,” she acknowledges.
“Fireworks are the trigger,” she says. “I know that’s going to be stressful. But if I can actually focus on the celebration of the freedom of America and refocus on the fireworks that will be in the air instead of my past experiences, it won’t be nearly as stressful and anxiety-triggering. I need to feel in control of my thought patterns because they automatically take me back to a dark and horrible time. I now have a tool I can use to refocus on what’s happening, instead of living in the past. Now, it’s the celebration. It’s happy, it’s good.
“What I won’t do is get drunk and pass out,” she adds. “What I won’t do is hide in my basement with earphones on. Now I can stay in my house, and it’s fine. I don’t have to drown it out. I don’t have to really get stressed out. It’s not 100%, but it’s not nearly as bad as it was.”
People with PTSD can have a number of distressing and persistent symptoms, including re-experiencing trauma through flashbacks or nightmares, emotional numbness, sleep problems, difficulties in relationships, sudden anger, and drug and alcohol misuse. Depression is one of the most prevalent mental health conditions found among Veterans and often co-occurs with PTSD.
In the coming weeks, Bean plans to take part in a William Marchand-led study focusing on equine services, or interaction with horses, as the complementary therapy.
“Dr. Marchand is a great instructor as far as meditation and mindfulness,” she says. “I saw his name and signed up because I think he’s a brilliant doctor. I would recommend his recreational therapies to other Veterans with PTSD.”
--- Mike Richman
VA Research Currents archives || Sign up for VA Research updates