Office of Research & Development |
 |
Office of Research & Development |
 |

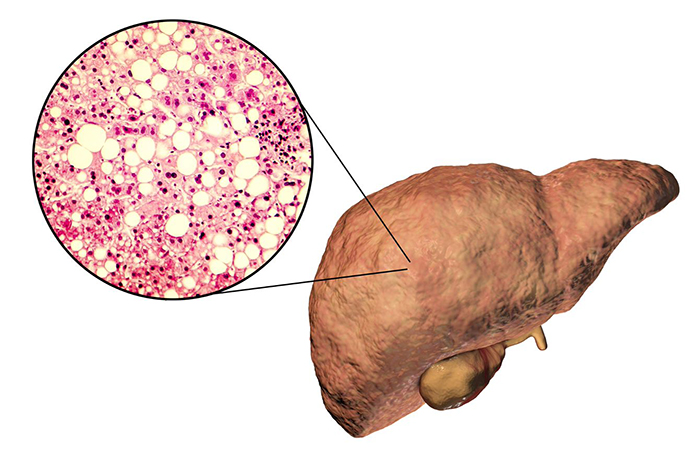
VA MVP researchers identified genetic risk factors for non-alcoholic fatty liver disease, a condition that can cause liver cancer and cirrhosis. (Image for illustrative purposes only. © Getty Images/Dr_Microbe)
July 6, 2022
By Tristan Horrom
VA Research Communications

VA researchers using AI to decide best treatment for rectal cancer

VA center training the next generation of researchers in blood clots and inflammation

AI to Maximize Treatment for Veterans with Head and Neck Cancer

VA investigator brings diversity into autoimmune disease research
A VA Million Veteran Program study identified genetic factors that increase the risk of non-alcoholic fatty liver disease (NAFLD). In a first-of-its-kind multi-ancestry genetic study, the researchers found 77 locations on the human genome that affect risk for NAFLD. Twenty-five of the locations had never been associated with the disease before.
The results can be used to build a genetic prediction model of NAFLD, according to the researchers, and will also increase understanding of how the disease develops.
The findings appeared in the June 2, 2022, issue of Nature Genetics.
The study involved over 90 VA scientists and their partner institutions. Drs. Kyong-Mi Chang and Benjamin Voight of the Corporal Michael J. Crescenz VA Medical Center and University of Pennsylvania led the study, along with first author Dr. Marijana Vujkovic.
The study exemplified the spirit of team science in MVP, notes Chang. "This study could not have been done without our Veterans’ altruistic participation in MVP to support scientific discoveries that can improve health care for other Veterans and the general public. In addition, strong support from the VA Office of Research and Development, MVP researchers, and their collaborators, made it possible to come together to study the growing global health issue of NAFLD,” she says.
NAFLD is defined as accumulation of at least 5% fat in the liver, in the absence of other known causes of liver disease. It can cause both cirrhosis and liver cancer. The condition has both genetic and biological risk factors.
NAFLD is a growing cause of liver disease due to a global obesity epidemic and associated metabolic disorders. It has an estimated worldwide prevalence of 25% in adults. In the United States, that prevalence is projected to climb to nearly 34% by 2030.
While NAFLD is a growing problem, it is markedly underdiagnosed because of the invasive nature of liver biopsies, high variability in imaging results, and poor sensitivity in diagnostic codes.
Because of the difficulty in diagnosing NAFLD, doctors often use a proxy method of identifying the disease. A blood test that checks for elevated levels of an enzyme called alanine aminotransferase (ALT) can be used to find NAFLD, along with medical history of risk factors such as obesity and diabetes. Chronic ALT elevation is a sign of liver damage.
To better understand the inherited risk for NAFLD, VA researchers studied the genomes of more than 90,000 MVP volunteers with chronic ALT elevation not explained by other factors. They compared this group to nearly 130,000 controls without elevated ALT. This was the largest genetic analysis to date using chronic ALT elevation.
The study population was particularly noted for being diverse, something not often seen in large genetic studies. The diversity of Veterans participating in MVP is an important strength of the program—MVP is one of the world’s largest and most diverse biobanks, with 25% of participants being non-white. This study population was 75.1% White, 17.1% African American, 6.9% Hispanic, and 0.9% Asian.
The researchers identified 77 locations on the genome across ethnicities where gene variation affected chronic, unexplained elevation of ALT. Of these, 25 had not previously been associated with NAFLD or ALT. They also identified one additional gene location associated only in participants of European ancestry, and two only in those of African ancestry.
The findings “effectively tripled” the known genetic locations related to NAFLD, according to Voight. “Genetic studies of NAFLD have been stymied owing to the difficulties and invasiveness of phenotyping patients,” he explains. “For the last 10 years, the total number of robust genetic associations known could be counted on two hands. That has been unquestionably frustrating.” This research adds greatly to the understanding of genetic risks for the disease, says Voight.
To verify the results, the team compared them to historical cases of NAFLD diagnosed by liver biopsy or imaging. Of the 77 identified gene locations, 17 were confirmed in the historical sample. All 17 of the replicated results and 61 of the 77 chronic ALT-associated locations have previously been linked to metabolic or inflammatory conditions. This suggests that metabolic disease and inflammation may be directly involved in the development of NAFLD, according to the researchers.
The research still falls into the “discovery” phase, according to Voight. As understanding of how genes affect NAFLD grows, research can help predict who is at highest risk for the disease, and subsequently which Veterans are likely to progress to liver cancer or cirrhosis.
Voight further explains that this human genetic data is crucial to success in drug development by providing new targets for therapeutic exploration. “Pharmaceutical companies have been extremely keen to leverage evidence from human genetics to guide development for a range of diseases, including NAFLD,” he says.
"Unfortunately, despite intense efforts, there is no effective FDA-approved treatment to date for NAFLD and its associated disease complications," explains Chang. "It is hoped that genetic discoveries related to NAFLD, such as those in this study, can lead to effective treatment for NAFLD and prevent liver disease progression. Genetic data may help in early identification of those with NAFLD who may or may not be at risk for liver disease progression to cirrhosis and/or cancer, so that such individuals can be monitored appropriately."
Future research will focus on using genetic data to examine shared genetic risk between NAFLD, liver cancer, and cirrhosis. “Finding a gene which relates to all three conditions and is also therapeutically actionably would be the ideal, dream scenario,” according to Voight. “To make that dream a reality, we are working to pull these pieces together.”
MVP is a national research program to learn how genes, lifestyle, and military exposures affect health and illness. Since its launch in 2011, over 875,000 Veterans have joined MVP, making it one of the world’s largest programs on genetics and health.
Voight expresses the importance of MVP in research, explaining, “The combination of the large number and diverse representation of participating Veterans allowing access to their extensive, longitudinal health records for research provides a truly unique and essential resource to advance our understanding of the genetic basis of human disease.”
Updated July 19, 2022.
VA Research Currents archives || Sign up for VA Research updates