Office of Research & Development |
 |


VA researchers studied how PTSD affects response to depression treatment. (Photo: ©iStock/junce)
August 4, 2020
By Tristan Horrom
VA Research Communications
The original VAST-D clinical trial included more than 1,500 Veterans with depression from 35 VA medical centers.
An analysis based on a large VA study on depression showed that patients with or without PTSD had similar relative responses to medication changes.
The original trial, the VA Augmentation and Switching Treatments for Improving Depression Outcomes (VAST-D) study, measured response in switching or augmenting treatment for patients not responding to antidepressants.

VA Researcher Named One of U.S.’ Top Female Scientists

Million Veteran Program director speaks at international forum
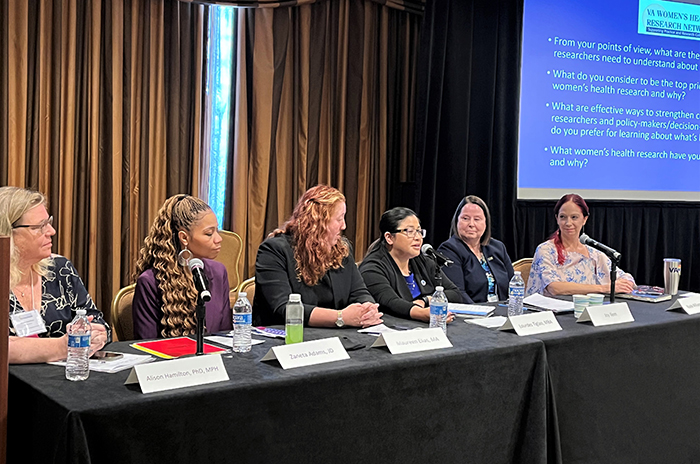
2023 VA Women's Health Research Conference

Self-harm is underrecognized in Gulf War Veterans
The new secondary analysis of this study group showed that participants who also had PTSD had generally worse rates of medication response, depression remission, and relapse than those without PTSD. However, different treatment changes yielded similar relative improvements in both groups.
VA researcher Dr. Somaia Mohamed, co-chair of the original VAST-D study and first author of the new analysis, notes that “VAST-D was the first study to show one treatment to have better results than others in the next step treatment of depression. The present secondary analysis extends these findings to show these differences in treatment benefits persisted when depression occurs with a specific psychiatric comorbidity.”
The results appeared June 23, 2020, in the Journal of Clinical Psychiatry.
PTSD and major depressive disorder frequently occur together, especially among Veterans. Previous research has shown that Veterans with both conditions have worse mental health outcomes than those with only one condition. But how PTSD influences the effectiveness of next-step medication for depression has not been widely studied.
To investigate this relationship, researchers from multiple VA health care systems performed a secondary analysis of VAST-D.
The VAST-D trial included more than 1,500 Veterans with non-psychotic major depressive disorder from 35 VA medical centers. At the time of enrollment, the participants were taking one of three common types of antidepressants: selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), or mirtazapine. For all participants, their current medication was not treating their depression effectively.
Participants were given one of three next-step treatments. Some were switched from their current medication to bupropion. Others had their current treatment augmented with buproprion. Buproprion is an antidepressant sold under several different names, such as Wellbutrin and Zyban. It can be taken on its own, but is also often used as a supplement to other antidepressants. A third group had the antipsychotic aripiprazole added to their existing treatment. Aripiprazole, sold under the brand name Abilify, is primarily used to treat schizophrenia and bipolar disorder.
In 2017, the initial VAST-D study found that augmenting with aripiprazole is the most effective next-step treatment for patients who are unresponsive to antidepressants.
The new analysis found that patients with PTSD had worse treatment response, remission, and relapse rates both before and after treatment change, regardless of the type of treatment they received: Adding aripiprazole led to depression improvement in 68% of patients with PTSD, compared to 79% of patients without PTSD. Switching to bupropion brought improvement in 58% of patients with PTSD and 67% of patients without PTSD. Treatment comparisons in the bupropion addition group were not significant.
However, while patients with PTSD were less likely to see improvements in depression, the changes in comparative effectiveness between different treatments were similar between patients with and without PTSD.
About 47% of participants in the VAST-D study had PTSD as well as depression. The original study analysis did not consider the presence of PTSD. This led to some concern that the large percentage of Veterans with co-occurring PTSD may have biased the results, favoring aripiprazole. The new analysis suggests that the conclusions of the VAST-D study hold true for people both with and without PTSD, according to the researchers.
“These results suggest that VA clinicians treating Veterans with both PTSD and major depressive disorder should discuss the possibility of augmenting their conventional antidepressants with aripiprazole,” concludes Mohamed.
The researchers on the new analysis were from the VA medical centers in West Haven, San Diego, Cleveland, Tuscaloosa, Tucson, Salem, Cincinnati, Asheville, and Philadelphia. The study also included researchers from the Yale University School of Public Health, and Baylor Scott & White Health.
VA Research Currents archives || Sign up for VA Research updates