Office of Research & Development |
 |


Veterans receive battlefield acupuncture treatment at the Washington DC VA Medical Center. An eye mask and soothing music in the background help create a relaxing environment. (Photo by Robert Turtil)
August 26, 2021
By Tamar Nordenberg
For VA Research Communications
"Pain is extremely prevalent among Veterans and others, and there is a need for novel pain treatment approaches."
During the Iraq and Afghanistan wars, a type of non-conventional therapy known as “battlefield acupuncture” (BFA) gained traction at Walter Reed Army Medical Center to treat the pain of wounded military men and women. “Western medicine was great for helping these patients but had its failures,” BFA originator retired Air Force Col. Dr. Richard Niemtzow wrote in an essay in the journal Medical Acupuncture. In recent years, VA has been integrating BFA—a type of acupuncture in which needles are placed on several specified points on each ear—as a choice for pain relief alongside conventional medications.
VA researchers have studied the therapy and published an article with their findings in the August 2021 issue of the journal Pain Medicine. The article, titled “The Implementation and Effectiveness of Battlefield Auricular Acupuncture for Pain,” discusses the promise and challenges of the approach.

VA opens new research center to seek novel arthritis treatments

Injectable gel could help treat degenerative back pain

Virtual reality technology helps Veterans in pain

Study outlines guidance for treating cancer patients who show a problematic pattern of opioid use
“Pain is extremely prevalent among Veterans and others, and there is a need for novel pain treatment approaches,” says VA’s Dr. Stephanie Taylor, the article’s lead author and the director of VA’s Complementary and Integrative Health Evaluation Center. “Not everything works for everybody. You need as many effective tools in the toolbox as you can get.”
Chronic (long-lasting) pain affects more than 50 million adults in the U.S., according to the Centers for Disease Control and Prevention (CDC). And chronic pain is more prevalent and intense among Veterans than among Americans generally. Medications have long been the mainstay of pain management. But these pharmaceuticals—including opioids, which are commonly prescribed for chronic pain—can be risky and have unwanted side effects. “I’ve spoken to so many Veterans who said they were on too many medications—more than 30, in some cases,” Taylor says. “They were looking for other safe and effective pain management options.”
In reducing Veterans’ pain while also lessening risk, VA offers battlefield acupuncture among other non-medication alternatives. These approaches can be used instead of, or along with, drugs. BFA is a type of auricular (ear) acupuncture that is based on the “meridian system” from traditional Chinese acupuncture. In BFA, health care providers place up to five sterile needles shaped like tiny darts in each ear at specific points. These points are believed to affect the entire body. The needles are meant to stay in the ears for several days. Precisely how the therapy works is unclear, but the needles may stimulate the central nervous system and reduce the sensation of pain by affecting parts of the brain such as the hypothalamus.
As discussed in the Pain Medicine article, BFA has been found to provide immediate, short-term reductions in pain for many. “It’s not a long-term fix,” Taylor emphasizes. “But for some people, it represents the first time in a long time they’ve had their pain reduced for even a moment.”
In Pain Medicine, Taylor and her coauthors summarize their research examining the effectiveness of BFA for pain relief. One study, led by VA’s Dr. Steven Zeliadt, examined more than 11,000 BFA users across VA.
The research found that a high proportion of patients benefited, with more than 75 percent of them reporting some immediate decrease in pain intensity after the treatment. In another study, a research team led by VA’s Dr. Dan Federman looked at patients attending an in-demand VA battlefield acupuncture clinic. The investigators found a decrease in pain in 82% of patients, on average, including patients seen in group settings and those seen in individual settings.
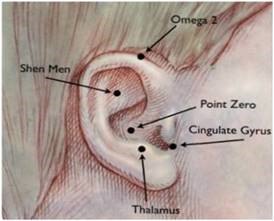 The five ear points used in battlefield acupuncture. (Illustration courtesy of Niemtzow, et al.)
The five ear points used in battlefield acupuncture. (Illustration courtesy of Niemtzow, et al.)
VA and the Department of Defense (DoD) both offer BFA for pain relief. In VA, the practice has been incorporated broadly. VA offers the therapy in a range of settings, such as primary care sites, pain clinics, physical therapy venues, emergency departments, and integrative care settings, such as chiropractic and acupuncture clinics. Battlefield acupuncture is easy to administer, and non-acupuncturist health care providers have been trained to deliver it.
VA and DoD have trained more than 4,600 health care providers to deliver the therapy, including doctors, nurses, nurse practitioners, physician assistants, chiropractors, occupational therapists, and physical therapists, along with licensed acupuncturists. VA is also helping the Indian Health Service train its health care providers in battlefield acupuncture.
As described in the Pain Medicine article, Taylor’s research team also conducted a study to learn about VA health care providers’ perceptions of battlefield acupuncture. Led by VA’s Dr. Karleen Giannitrapani, they conducted phone interviews with many BFA providers.
Those interviewed cited the following perceived advantages of BFA:
Providers perceived these to be among the disadvantages of BFA:
The authors recognize the nascent clinical evidence to be among the major challenges to BFA acceptance. Prior to the studies Taylor and colleagues discussed in Pain Medicine, only three small studies had been conducted of the emerging treatment approach. The VA researchers concluded that additional, rigorous, longer-term research is needed so the treatment and its effectiveness can be better understood.
Meanwhile, some BFA supporters who were interviewed in the phone research said they won trust for BFA from hesitant facility leaders and patients by encouraging them to personally observe or experience the technique.
Patients who have experienced BFA treatment have been shown to subsequently try traditional acupuncture, as well. As described in Pain Medicine, a study by Taylor’s team led by VA’s Eva Thomas, found that patients who used BFA had more than 10 times the chance of using traditional acupuncture within the following three months, compared to the general population.
Also, the immediate, short-term relief from BFA “may provide a ‘window’ to allow some patients to engage in other, more long-term approaches, such as yoga and tai chi,” according to the article in Pain Medicine, “ultimately moving toward more of a self-management model to address their chronic pain.” These types of integrative and complementary forms of health care are the foundation of a budding personalized approach to care at VA known as “Whole Health.”
The Whole Health program is based on each Veteran’s values, needs, and goals. As for Taylor, researching these integrative and complementary approaches is her “passion,” she says, “because it is important to offer Veterans evidence-based, non-pharmacological pain management options.”
VA Research Currents archives || Sign up for VA Research updates