Office of Research & Development |
 |
Office of Research & Development |
 |


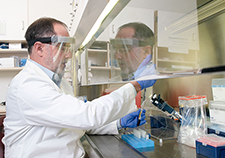
Dr. Karin Nelson is a primary care physician and researcher at the VA Puget Sound Health Care System. (Photo by Christopher Pacheco)
November 13, 2019
By Mike Richman
VA Research Communications
"Our results provide a starting point for understanding and maximizing the clinical utility of predictive indexes in routine practice."
As a VA primary care clinician, you’re seeking information on patients who are at the greatest risk of hospitalization or death within a year. What resource do you turn to?
One option is the Care Assessment Needs (CAN) report, a form of predictive analytics. It looks at factors such as vital signs, lab results, doctor and pharmacy visits, emergency room use, and coexisting conditions to calculate a risk score. Specifically, the score shows how likely a VA patient is to end up in the hospital or to die within a given time period, such as 90 days or a year. The score also compares the Veteran with others and ranks them from lowest to highest risk.
VA developed the CAN report in 2012. Depending on its assessment, the report may be a starting point for clinicians to consider referring patients to intensive outpatient care, such as nurse-managed home care or palliative services. The latter approach is meant to improve the quality of life for patients and their families facing physical, social, and spiritual problems associated with a life-threatening illness. The report does not suggest drugs to prescribe or assess the need for surgery.
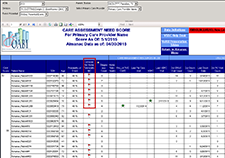
A sample screenshot shows what VA primary care providers see when they access the Care Assessment Needs (CAN) report.
Dr. Karin Nelson, a primary care physician at the VA Puget Sound Health Care System in Seattle, led a study that examined how many primary care clinicians and nurses use the CAN score and sought their suggestions for improving the tool. The results appeared in the Journal of General Internal Medicine in August 2019.
Nelson and her team determined that the extent of CAN score use among more than 8,600 primary care providers and nearly 6,500 nurse care managers in VA varied widely by clinic. During the three-month survey period, the researchers found an average of nearly 6,500 uses of the CAN report among an average of 1,850 users. The users received an online survey. Most of the 400 respondents viewed the CAN score favorably across a series of measurements:

AI to Maximize Treatment for Veterans with Head and Neck Cancer
VA Further Develops Its Central Biorepository: VA SHIELD

VA research being used to help children with heart defects
In qualitative answers, the respondents indicated that the CAN scores were often used for care coordination or palliative services. At the same time, they expressed a need for more help in using the score and noted that like other forms of predictive analytics, the CAN score results weren’t always clinically actionable.
“A lot of these kinds of risk scores don’t suggest a clinical follow-up,” says Nelson, who is also a professor at the University of Washington. “You might know that the patients are at high risk just by virtue of their medical condition. But that doesn’t necessarily point you to the next step that you should take with the patient. So the score really indicates the risk, but it doesn’t point out the next step in clinical care.”
The respondents also called for the CAN report to be integrated into VA’s electronic health record—the Computerized Patient Record System. Currently, those seeking access to the CAN dashboard only have the option of going to two internal VA web sites separate from the electronic health record to find the CAN scores and information on high-risk patients: the Primary Care Almanac and the Patient Care Assessment System. In Nelson’s view, having to do that likely dissuades some providers from accessing the CAN dashboard.
Both sites allow teams to assign clinical priority and urgent flags that are based on the CAN score and other clinical criteria. The new version of PCAS produces a note to send to the electronic health record that includes all of a patient’s CAN scores.
“You’re less likely to use the CAN score when you’re talking to a patient because you have to go and find it somewhere else,” Nelson says. “You have to take extra time to search for it. So it’s more for panel management when you’re not with patients. Having the CAN score and other decision aids integrated into the medical record would help providers identify and treat their high-risk, high-need patients.
“Right now, if I pull up a patient’s name, I can’t see that person’s CAN score,” she adds. “I have to go to another dashboard and log into another report. That’s pretty similar to a lot of other VA reports, such as the diabetes registry. A lot of VA’s online dashboards are separate from the electronic health record. They include data from the Computerize Patient Record System. But they’re not readily available when looking at a patient’s chart. Like with anything, if you have information that’s easier to find, you might actually use it more.”
The CAN scores haven’t been integrated into the electronic health record because of a long-standing VA policy that prevents the introduction of new features to the system while another one is being developed. VA is in the process of transitioning to the Department of Defense’s electronic medical records system to allow for seamless care between the agencies. The new platform is commonly called “Cerner,” the name of the health technology company that developed it.
Nelson uses the CAN report to see which patients have had multiple emergency room visits and who could potentially need referral to home telehealth or palliative care. “It’s a case-finding tool,” she says. “So in that regard it’s successful because it does find those people.”
Dr. Tami Box, director of clinical systems development and evaluation at VA, says several steps are required to ensure the integration of models like CAN into Cerner. They include the creation of an interface for Cerner to receive the CAN scores and validation of the new Cerner data as facilities go live to ensure that the data function properly in the models.
“To that end, our team is working directly with Cerner and key VA leaders to specify the data required for the CAN scores and ensure those data are a priority for syndication to the initial sites that are testing the new electronic health record system,” Box says. “In the meantime, we will continue to maintain the weekly CAN score production, the CAN dashboard, and the use of the CAN scores across VA in applications like the Patient Care Assessment System.”
“VA has a robust history of developing important metrics, models, and other tools that would be maximally useful if they could exist in the context of clinical care,” she adds. “Namely, they should be directly available in the health record at the point of care to help guide clinical management and treatment. We hope a modernized records system with appropriate interface opportunities could facilitate this for models like CAN.”
One of VA’s other risk scores assesses a Veteran’s chances of suicide and opioid overdose. That score is also not integrated into VA’s electronic health record.
In terms of her study, Nelson says she wasn’t “too surprised” the respondents couldn’t always put the CAN score results into action in a clinical setting.
“That was not surprising because I’m a practicing physician, and that’s what I think,” she says. “I’m not surprised when I look at my list of patients with CAN scores with the highest probability of hospitalization or death. But the fact that they’re high-risk doesn’t always help me with what to do for them because people are so complicated and there are many different reasons they have this high risk. It’s challenging to take care of patients with these risks.”
Nelson and her colleagues caution that the findings in the study are “preliminary and limited” by a low survey response rate of 400 people. They also say there may have been a response bias in the study, in that providers more familiar with CAN may have been more likely to complete the survey than those who use the system less often.
“Nonetheless, our results provide a starting point for understanding and maximizing the clinical utility of predictive indexes in routine practice,” the researchers write. “The CAN score is being applied in a number of quality-improvement projects and research studies with the goal of learning not only the effectiveness of intensive management for these patients but also the clinical processes needed to make use of CAN score information.
“The CAN score illustrates how a health care system can harness electronic health record data to identify high-risk patients who may benefit from clinical interventions,” the researchers add. “Additional work is needed to fully [assess the diversity] of these patients’ needs, and to determine the best methods for using the score to target patients in need of specific services.”
VA Research Currents archives || Sign up for VA Research updates