Office of Research & Development |
 |

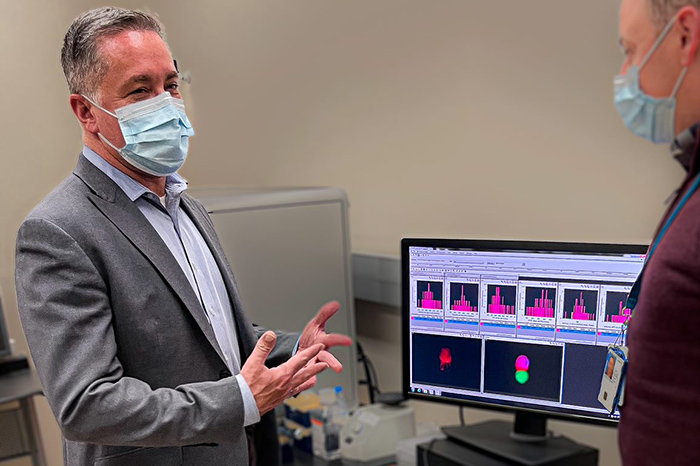
As the director of VA Eastern Colorado, Michael Kilmer (left) oversees one of the largest Veteran populations of any VA medical center. (Photo by Teresa DiBella)
November 18, 2021
By Mike Richman
VA Research Communications
After earning a master’s degree in social work and mental health from the University of Washington in 2004, Michael Kilmer began his first stint in VA at the VA San Diego Healthcare System. A Coast Guard Veteran, he worked there for four years, creating a nationally recognized care management program for post-9/11 combat Veterans.
In this role, Kilmer assisted Dr. Dewleen Baker, a prominent psychiatrist and researcher with a concentration in neuroscience. He evaluated transitioning Veterans by carrying out psychological and psycho-social assessments, and he co-authored studies led by Baker on mental health factors related to this population.
"It saddens me when I see clinical and research being on opposite sides of the aisle, if you will. Everyone wins when they work together."
At the time, Kilmer recalls, Baker ingrained in him a philosophy that he takes to heart today as director of the VA Eastern Colorado Health Care System: Good clinical work supports good research, and good research supports good clinical work.
“They really are hand in glove,” Kilmer says. “She taught us about the importance of having the support of evidence-based assessment tools. By using these tools and documenting [the research] in our clinical work, we were able to produce some amazing literature. I’ve always seen the benefit of research and clinical working together. That’s been true my entire career. It saddens me when I see clinical and research being on opposite sides of the aisle, if you will. Everyone wins when they work together.
“In some facilities, I’ve seen a lack of understanding of one side of the house or the other,” he adds. “I’ve seen a lot of directors that put a priority only on access to clinical care. That’s incredibly short-sighted in the long run because clinical and research work together. You need the right balance. We have four missions: clinical, research, academic, and emergency management. They all need to work together.”

VA center training the next generation of researchers in blood clots and inflammation

AI to Maximize Treatment for Veterans with Head and Neck Cancer

VA researcher works to improve antibiotic prescribing for Veterans
VA’s Million Veteran Program played crucial role in nation’s response to COVID-19 pandemic
The motto that Kilmer acquired from Baker, who is now the research director at the VA Center of Excellence for Stress and Mental Health at VA San Diego, is one that she still upholds.
“I’m delighted that he took it up to that degree,” Baker says. “I’m thrilled that he has carried this forward because I think it’s critical for good clinical treatment. Michael has always been very friendly to research and finding a way to make it clinically useful.”
Championing research is one of Kilmer’s fundamental priorities at VA Eastern Colorado, which employs more than 3,400 health care professionals. The hospital, which is based near Denver in the city of Aurora, also oversees one of the largest Veteran populations of any VA medical center—about 100,000—in a region covering a wide swath of eastern Colorado and neighboring states. Plus, VA Eastern Colorado maintains one of the biggest annual budgets for a VA medical center, at $835 million.
Kilmer came to VA Eastern Colorado in September 2019, after serving in the same role at VA Grand Junction, a much smaller facility in the western part of the state. His orientation period at VA Eastern Colorado was relatively brief, before an emergency set in.
Toward the end of the holiday season, the World Health Organization learned of pneumonia cases from an unknown cause that were detected in Wuhan, China. Word subsequently spread about a mysterious virus rapidly taking hold in parts of the world, including the United States. Kilmer and his colleagues at VA Eastern Colorado closely monitored relevant developments in Italy, which became a hotspot for the novel coronavirus, as well as the port cities of New York and Seattle, where the first case of the COVID-19 was detected in mid-January.
Denver, Kilmer notes, was projected to be a “second wave city.” He and his staff developed a plan to convert from normal operations to potentially providing full COVID inpatient services, with a surge from 88 medicine, surgical, and ICU beds to 346. To realize such a sharp increase, he says, the hospital doubled up many rooms and reallocated other units, such as inpatient psychiatry and spinal cord injury.
“For Seattle and New York, it was more like being hit by a tornado, but we saw a hurricane coming,” Kilmer says. “We had more time to strategically plan and operationalize our plans. It was truly impressive to see how everyone worked together. Seeing the images of what was happening in Italy, Seattle, and New York, we had an internal mantra of no one on the floor. In the early days of COVID-19, people were looking at images of patients on the floor in the waiting rooms. So no one on the floor, the safest care possible, and as few deaths as possible. Those were our three goals because it was emergency managing.”
With COVID-19 in mind, Kilmer dubs himself a “big believer of not letting a good crisis go to waste.” He’s pushing for his researchers to generate streams of studies related to the pandemic. The hospital is now funding 26 studies through its COVID-19 budget, including studies on COVID in the brain, the effectiveness of COVID medications, the nutritional impact of the virus on Iraq and Afghanistan Veterans who have had traumatic brain injuries, and the effects of COVID and social distancing on mental health.
Some of the investigators have deviated from their normal research to focus entirely on COVID. For others, the theme of their studies is rooted in the foundation of their ongoing research.
During the early days of the COVID crisis and beyond as the director of VA Eastern Colorado, Kilmer has employed leadership and managerial skills that he honed during his 15-year stint in the U.S. Coast Guard (1987 to 2002). His military career was split between operational duties and human resources.
Kilmer spent three years on the Coast Guard cutter Munro based in the San Francisco Bay area for war-time readiness, search and rescue, and law enforcement operations, among other necessities. For six months, he took part in Operation Deep Freeze, an ongoing U.S. military mission to resupply bases in Antarctica. He spent the rest of his time in support roles.
In his current position, Kilmer lives by the Coast Guard values of honor, respect, and devotion to duty. He believes his Coast Guard operational duties prepared him the most for being the director of a VA medical center. That’s because in Coast Guard operations, he says, “You’re always asking do you have the right people with the right training and the right equipment in the right place at the right time. That foundation is very similar to running a health care system.
“As far as leadership goes, it’s so critical that you prepare your staff to meet the challenges,” he explains. “With a shared vision, goals, and a common operational picture, you ensure your team has resources, and you can let them go to accomplish the mission. I believe more in the values of servant leadership than being a micromanager.
“If you look at how our team stood up during the [COVID-19] emergency, it could have been two different scenarios. We could have had centralized command and control, with top-down decisions, but we didn’t do that. My Coast Guard experience taught me to lead and support a team from a unity-of-effort framework because our health care system is so complex. We also had to consider our coordinating efforts with local, state, and other federal agencies. That added an extra layer of complexity. These complexities enforced the need for shared purpose and a mindset of unity of effort, because no one person or agency can know or do everything.”
Kilmer has steered a number of big vessels in his VA career. Following his experience at VA San Diego, he worked for the Veterans Health Administration overseeing multidisciplinary care management across southern California and southern Nevada, before being promoted to VA headquarters in Washington in 2013. He later served as interim director of the Amarillo VA Health Care System in Texas and the Central Texas Veterans Health Care System. He became the director of VA Grand Junction in April 2017 and remained in that role for more than two years.
In transitioning from VA Grand Junction to VA Eastern Colorado, Kilmer went from what he calls “more of a community and critical access hospital” that is centered mainly on primary care, to a VA medical center that provides most levels of care. In addition to the primary hospital, VA Eastern Colorado oversees the Rocky Mountain MIRECC (Mental Illness Research Education and Clinical Center) for Suicide Prevention, a Geriatric Research Education and Clinical Center (GRECC), and the Center of Innovation for Veteran-Centered and Value-Driven Care, as well as six CBOCs (community-based outpatient clinics), two primary care telehealth outreach clinics, and a community living center, among other satellite facilities.
VA Eastern Colorado also has a strong academic affiliation with the University of Colorado and supports more than 164 medical residents and over 400 allied health professionals.
“Being in Grand Junction in a small, very supportive community, it was more like being the commanding officer of a fast frigate,” he says. “Whereas at Eastern Colorado based in Aurora, with our amazingly beautiful and very high-tech medical center, it’s more like being the admiral of an aircraft carrier with its entire fleet.”
In Dewleen Baker’s opinion, Kilmer’s “huge” leadership skills existed well before he came to VA, as well as his special touch when working with patients.
“I tend to provide what a patient needs, even if it’s a little outside of my specific psychiatry role,” she says. “If somebody needs something, I’m not going to have them call me and not respond, for example. Michael was very much the same way. First of all, he has huge insight into patients and a great rapport with patients. I always knew if I gave him somebody to work with, or I had somebody who I referred to him, I never had to worry. He was going to take care of that person, and he did a wonderful job. Administratively, from my point of view, he made great decisions. I’m not at all surprised that he’s moved up the ladder.”
In the coming months, every VA medical center in the country is expected to have access to eScreening, a mobile electronic program in which patients can enter mental and physical health data about themselves. It identifies early health problems and expedites the process in getting newly enrolled Veterans to the appropriate mental health and psychosocial services, while proving to be feasible, efficient, and cost-effective.
Previously, screening was accomplished through the cumbersome process of a patient filling out paper forms in pen or pencil, and a clerk typing this information into the Veteran’s electronic health record.
The eScreening option likely wouldn’t be as ubiquitous without the foresight of Michael Kilmer.
A little more than a decade ago, Kilmer, now the director of VA Eastern Colorado (see main story), worked as a specialist in social work and mental health at VA San Diego alongside Dr. Dewleen Baker, a renowned psychiatrist. The two envisioned eScreening as a way of carrying out research assessments to support clinical work. Kilmer also helped gain the funding for the project after coming in contact with representatives from a small tech company applying for a VA IT Innovation Grant.
“The company approached me with some ideas of how it could assist in improving clinical services, and they needed a VA medical center to partner with,” Kilmer recalls. “We dove into our comprehensive biopsychosocial screening and assessment process and considered how we could move it from pencil and paper to an electronic platform. My idea was to transform the clinical-research assessment into an electronic and automated process that was integrated with our electronic medical records for an easy and effective process. That was the birth of what we now know nationwide as eScreening.”
In Baker’s opinion, eScreening never would have happened without Kilmer’s introduction of the IT company to Dr. James Pittman and Dr. Niloofar Afari, members of the VA Center of Excellence for Stress and Mental Health (CESAMH) at VA San Diego. “Michael was totally instrumental” in the evolution of the program, Baker says. The funding, she explains, enabled Pittman and Afari to build the eScreening infrastructure for local use and establish its benefits for Veteran care. Their efforts to implement eScreening have led to a national rollout to VA facilities, which CESAMH is helping carry out.
Similar systems exist in the private sector. But VA built eScreening before anything like it was implemented in a private health care setting, according to Pittman. Plus, eScreening can be customized for program needs without the use of a software engineer and has two-way communication with VA’s Computerized Patient Record System (CPRS), which houses Veterans’ electronic health records. It also provides feedback to Veterans to help facilitate health conversations. Those features separate it from anything in the private sector, Pittman says.
Today, eScreening is available at 25 VA medical centers and should be in all VA facilities by March of next year. Pittman says software deployed to every facility in the country will allow the eScreening program to communicate with the CPRS. The program allows Veterans to report all types of health information that ends up in their electronic health record, including physical, mental, social, and service preferences, and that VA researchers and clinicians can review. The eScreening program, Kilmer notes, has been so effective that VA Eastern Colorado has hired a staff member to implement it across the facility’s vast health care system.
“Early identification and intervention of a Veteran’s mental health care needs is the vision of eScreening,” he says. “The eScreening option, while easy and effective to use, demonstrates how we can use evidenced-based screening and assessment tools in both research data collection and direct clinical services. It’s also a great example of research and clinical professionals working hand-in-hand together.”
Early on, Baker says, eScreening was only available on an Ipad when a patient would come to a VA hospital. Now, Veterans can enter information into the system on their home computer. The program is also being used with informed consent, she adds, to collect data that are being integrated into a biorepository to track symptoms and potential biological markers.
“There are various ways eScreening can be used in conjunction with research and clinical needs,” Baker says. “It makes information much more readily available to clinicians, so it’s broadly useful.”
--- Mike Richman
VA Research Currents archives || Sign up for VA Research updates