Office of Research & Development |
 |


More than 60 VA medical centers have been involved in trials on COVID-19 therapeutics, including antiviral drugs such as remdesivir, monoclonal antibodies, convalescent plasma, and immunomodulators. (Photo for illustrative purposes only: ©iStock/andresr)
January 3, 2022
By Mike Richman
VA Research Communications
"There's great scrutiny over COVID-19 research because it's a new illness in humans and because the research world is moving so quickly to develop tools to fight it."
Since the start of the COVID-19 pandemic, VA has played a critical role among federal agencies in the study of drugs or other therapies needed to treat patients with the virus.
VA has been part of major national research initiatives on COVID-19 vaccines and therapeutics, including Operation Warp Speed, which is now the Countermeasures Acceleration Group, and the ACTIV initiative. ACTIV is an NIH-created public-private partnership aimed at developing coordinated research strategies among federal agencies for prioritizing and speeding the creation of the most promising COVID-19 treatments and vaccines. In addition to federal agencies, ACTIV includes representatives from academia, pharmaceutical companies, and philanthropic groups.
Currently, VA researchers are contributing to preclinical activities in the ACTIV initiative by identifying emerging viral mutants. VA is also partnering on five ACTIV clinical trials: ACTIV-2, ACTIV-3A, ACTIV-3b, ACTIV-3c, and ACTIV-4a. In these trials, COVID treatments are studied for effectiveness and safety. The trials are stopped quickly if the therapies being tested are found to be ineffective, or if safety concerns arise. But if promising data emerge, the trials will continue and new agents may be added, all within one clinical trial.
To date, more than 60 VA medical centers have been involved in trials on COVID-19 therapeutics (see sidebar), including antiviral drugs such as remdesivir, monoclonal antibodies, convalescent plasma, and immunomodulators. Other therapeutics are in the pipeline for clinical trials, but only one has received FDA approval.
In August 2020, VA launched a master protocol program called VA CURES that aims to give Veterans faster access to potential COVID-19 treatments and to test their effectiveness. The initiative has led to a series of clinical trials across the VA network. As a master protocol, VA CURES offers a standardized framework for studies on many potential treatments for COVID-19, without the need for a new study design and protocol each time.

AI to Maximize Treatment for Veterans with Head and Neck Cancer

VA researcher works to improve antibiotic prescribing for Veterans
VA’s Million Veteran Program played crucial role in nation’s response to COVID-19 pandemic
VA Further Develops Its Central Biorepository: VA SHIELD
VA CURES has developed into a clinical trial site network that is participating in one of the ACTIV trials. This network brings clinical trial infrastructure and expertise for supporting infectious disease trials.
For more on VA’s role in identifying COVID-19 therapeutics, VA Research Currents spoke to three experts in VA’s Office and Research and Development (ORD): Dr. Molly Klote (MK), Dr. Victoria Davey (VD), and Dr. Terri Gleason (TG).
VA Research Currents: What factors make VA a good place to conduct studies on COVID therapeutics? Electronic health records? Diverse patient population? Geographic diversity? Investigators and teams experienced in infectious disease?
TG: All of those factors are important to characterize why VA is a good place to conduct clinical trials to find solutions to COVID-related care. VA’s mission especially supports the rationale and philosophy to advance health care and Veterans for the nation. From the earliest days of the pandemic, VA research scientists across the country focused directly on how we can help drive the solution set for anyone impacted through sound scientific research.
MK: The best reason to conduct therapeutic studies in VA is because of our population. All of the reasons stated above are good practical reasons, and we have amazing relationships with our federal partners. But the primary reason VA is a great place to conduct clinical studies is we have a patient population that is invested in their care and the advancement of science for their own health and the health of their fellow Veterans. This is a population that volunteered to protect our nation, and they continue to volunteer to change the world of health and health care.
VD: I’ll add that a huge factor is the dedicated investigators and teams who are very determined to find tools to stop this pandemic, ultimately so that we can better care for Veteran patients. To that end, we’ve had investigators with infectious disease training join the ACTIV trials, but also general internists, cardiologists, pulmonologists and oncologists—VA staff and their teams with research credentials in other disciplines. The broad background of these investigators has made COVID therapeutics research well-rounded and considerate of many aspects of Veterans’ short- and long-term health. Simply put, VA has all the necessary components to do this work and more. A number of factors are required to be successful in research, and VA has the experience, tools, and people to help provide quality evidence for research on COVID and COVID therapeutics.
Has VA built new infrastructure to enable research on COVID therapeutics, such as centers, funding mechanisms, or collaborations?
TG: VA research has increased infrastructure investments related to support for COVID research, including in new funding opportunities, new clinical trial networks, advanced data centers and programs, and biorepository resources. From small to large endeavors and new established federal partnerships, VA research has been highly focused on collaborative well-informed infrastructure and funding opportunities.
We also established VA CURES, which has evolved into a clinical trial network. Starting with the first partnership on ACTIV4a, the VA CURES network has been an important pathway for trials focused on infectious diseases, including COVID-19 therapeutics, and will serve as an attractive resource for partnering with other federal agencies who find a large VA clinical site network a true advantage for completing multi-site trials.
VD: We’re also in mid start-up of a fantastic resource—a national VA biospecimen repository called VA SHIELD. It’s a federated system of physical biorepositories to which any VA site can contribute remainder specimens, such as nose swabs done for diagnostics that have no more use for the clinicians but are a source of the virus that can be genetically sequenced to track mutant strains. VA SHIELD should develop over time to be a center of biospecimen storage, with the ability to join specimens with donor data, while protecting privacy and confidentiality. This is another way we have been able to use COVID-19 to achieve long-term goals in VA research. VA leverages its resources, including a national clinical research enterprise. As a program with its own congressional appropriation, VA also is able to support new requirements that are specific to COVID.
MK: We have joined the NIH-created ACTIV initiative and are contributing to basic, clinical, and prevention research. For the ACTIV-2 and ACTIV-3 studies, we put together a coordinating center for the collaboration with the National Institute of Allergy and Infectious Diseases (NIAID) and its international infectious disease trial networks. This network has a long productive history of clinical research in HIV and influenza. But at the start of the pandemic, NIAID reached out to other networks to join forces, including VA, thinking we are better off collaborating strategically than developing separate research initiatives. In addition to ORD support, we established a memorandum of understanding with NIAID for current and future research and an interagency agreement for work on ACTIV studies.
Are there new partnerships that have arisen to support the study of COVID therapeutics?
TG: Many new partnerships have arisen specifically as a result of the need to find therapeutic and prevention solutions for COVID-19. For therapeutics, VA developed VA CURES to support ORD clinical trials, for example, by studying the benefits of convalescent plasma. VA CURES has evolved into a clinical trials network to support trials with other federal partners.
Partnerships with NIH and NIAID were referenced earlier. Additionally, VA has been collaborating with NIH, the Food and Drug Administration (FDA), the Centers for Disease Control and Prevention (CDC), and the Department of Defense (DOD) to gain a fuller picture of the extent of COVID-19 outbreaks and affected patients, to conduct analyses looking at vaccine and treatment effectiveness, and to identify opportunities for further study by knowing the types of data being collected for analysis.
Editor's note: In July 2020, VA began collaborating with the Department of Energy (DOE) and the Department of Health and Human Services (HHS) on an initiative called the COVID-19 Insights Partnership. The endeavor creates a framework for VA and HHS to use DOE's high-performance computing and artificial intelligence resources to conduct COVID-19 research and analyze health data that would otherwise not be possible.
Has COVID-19 raised VA’s visibility or prestige—both in the public and among federal and industry partners—because of the agency’s contribution to developing therapeutics and assisting in evaluating vaccines?
MK: We hope the nation has seen the tremendous return on investment in the VA clinical and research enterprise. VA has been a major force in the fight against COVID-19. We opened our medical center doors to handle the overflow from non-VA facilities and were able to shift staff through our volunteer staffing process all across the country wherever the pandemic was surging. We joined with the DOE, DOD, and NIH in the fight through Operation Warp Speed, and we feel that those agencies now have a new appreciation for our inherent strengths as a health care and research system.
VD: VA has been able to contribute to the understanding of COVID-19, as well as treatment and prevention efforts. We have been lauded for our work with the NIH ACTIV Tracking Resistance and Corona Virus Evolution (TRACE) initiative. That’s not only for contributing data on viral sequences infecting Veterans but also for donating COVID-19 convalescent sera of Veterans who’ve been vaccinated with approved vaccines for further study of the relationship between vaccination and the development of coronavirus mutants.
VA has always been a national leader in biomedical research, with many firsts and demonstrated abilities to conduct impactful research. During the pandemic, VA has played a key role in high-visibility studies and has helped to coordinate activities using the VA health care system as a platform for better understanding the coronavirus, its effects, and treatments for it.
How do we go about enrolling patients in therapeutic studies who are very ill, say in the ICU? Do their families generally sign the consent forms? Do they need to have already filled out legal forms authorizing their families to act on their behalf?
MK: Federal regulations allow for situations where a patient may not be able to provide self-consent. Of course, our preference is always to get consent from the patient. In those instances when that's not possible and there's a proposed benefit to the study interaction with an appointment or counseling or to treatment with a therapeutic drug or device, we turn to the patient's legally authorized representative (LAR) for consent. Once the patient is again able to provide self-consent, that person is offered the opportunity to stay in the research study or withdraw. Different states have different rules regarding who can serve as the LAR. A medical power of attorney is generally allowed to serve in this capacity, but that designation is not required in writing.
TG: Early pandemic VA trials were focused on enrolling patients mostly from the ICU. Research teams quickly developed appropriate informed-consent procedures by working with local and central oversight committees, as well as with faculty staff, such as nurses, to collaboratively set up acceptable processes in an ICU setting. In addition to the LAR process, teams made use of technology to manage safety requirements, with paper versus electronic capture, electronic document signing, and other means.
What can you tell a patient about the safety and protection inherent in these trials?
MK: All clinical trials are subject to the peer review of the science of the study, then an ethical review as to the risk and benefit to the patients to be enrolled. Part of that ethical review involves ensuring that there is a plan to closely monitor the study participants and to make sure they are notified if there are any changes to the risk benefit from what they were told when they first enrolled in the study. Each year, or sooner than that depending on the risks of the clinical trial, the institutional review board (IRB) made up of scientists, non-scientists, and community members reviews the progress of the study and decides if the study can still go forward. Some studies require a data safety monitoring board, in addition to the IRB. The IRB reviews the results of that group, which focuses solely on the safety data.
TG: The risks and benefits of participating in a clinical trial are described in the informed-consent process. The informed-consent information is approved by oversight committees before it is presented to a potential research volunteer. In the case of the quickly changing and evolving scenario from the pandemic, information about effectiveness is challenging to convey. However, a study participant is always presented with a choice of volunteering to participate in a study. Additional safety review of a trial and its accumulated data on adverse events are also subject to data-monitoring reviews for the protection of participants.
VD: Some of our ACTIV trials are being reviewed by data safety and monitoring boards every two weeks. Their reports then go to their IRBs for additional review. There’s great scrutiny over COVID-19 research because it’s a new illness in humans and because the research world is moving so quickly to develop tools to fight it.
Hypothetical scenario: Someone shows up at a hospital and tests positive for COVID. How would staff go about approaching that person regarding a clinical trial?
MK: Investigators may present options for research studies to the patient in the language of the patient’s choosing and answer as many questions as necessary until the patient feels that he or she has enough information to make an informed choice. Sometimes, like with COVID-19, there are no other options for treatment. The investigator will be open and honest about that, as well.
Are there areas in COVID therapeutics where the guidelines are ambiguous or open-ended, and where VA has needed to come down on one side or the other in terms of whether to prescribe a certain treatment?
VD: In the U.S., our medical system is open to the fact that many organizations can write clinical care or practice guidelines. These guidelines come from government agencies like NIH and from other agencies or departments that represent special populations like active-duty military or Veterans. VA has developed many practice guidelines for conditions or diseases of special concern to Veterans, such as hepatitis C. Professional specialty medical societies develop guidelines, too. Some guideline committees are very well-known with COVID-19, such as the CDC's Advisory Committee on Immunization Practices, which advises and guides the CDC director on recommendations for the use of vaccines.
The FDA makes new treatments available through its emergency use authorization process, a culmination of deliberations and determinations by science and policy experts for a 'best' path forward when there is still uncertainty. For COVID-19, NIH rapidly developed and modified treatment guidelines that are widely followed but not mandated. VA will sometimes create policy or recommendations to follow others' guidelines—such as the NIH COVID-19 treatment guidelines—and make decisions via expert committees that report to the VA under secretary for health. But, as there is much in COVID-19 that is ambiguous, clinicians use guidelines, as well as their knowledge and experience, to treat patients.

Photo for illustrative purposes only: ©iStock/digicomphoto
Drug name: remdesivir (brand name Veklury)
Type of drug and what it does: Remdesivir is an anti-viral drug that works by stopping COVID-19 from reproducing and spreading through the body.
FDA approval status: approved
Which COVID patients receive it: Remdesivir is for adults and certain pediatric patients (12 years of age or older and weighing at least 88 pounds) with severe COVID-19 who are sick enough to need hospitalization. The FDA says remdesivir should be administered only in a hospital or health care setting capable of providing acute care comparable to inpatient hospital care.
VA role, if any, in research on the treatment: The VA medical centers in Denver, New Orleans, and Palo Alto took part in a randomized, placebo-controlled study on remdesivir led by the National Institute of Allergy and Infectious Diseases. Trials of the drug have showed that it can cut recovery time by nearly a third in people with severe COVID-19.

Photo for illustrative purposes only: ©iStock/digicomphoto
Drug name: baricitinib (brand name Olumiant)
Type of drug and what it does: Baricitinib is an anti-inflammatory used to treat rheumatoid arthritis, a chronic condition characterized by joint inflammation. It also has antiviral ability and is in the JAK class of immunomodulators, which support immune function by modifying, in a beneficial way, the immune system’s response to a threat.
FDA approval status: emergency use authorization (EUA)
Which COVID patients receive it: Per the FDA’s updated EUA in July 2021, baricitinib can be given for treating severe COVID-19 in hospitalized adults and children two years of age or older requiring supplemental oxygen, non-invasive or invasive mechanical ventilation, or extracorporeal membrane oxygenation, a form of life support. Previously, baricitinib was authorized only if given with remdesivir, according to the FDA’s original emergency use authorization in November 2020.
VA role, if any, in research on the treatment: VA researchers have participated in two trials on baricitinib. In one study, 15 patients with moderate to severe COVID-19 received daily doses of baricitinib, in addition to their background treatment. The combination was linked to the recovery of 12 of the patients. In the other trial, although there was no major drop in the frequency of disease progression overall, treatment with baricitinib in addition to standard of care was similar in safety to that of standard of care alone and was linked to lower death rates in hospitalized adults with COVID-19.

Photo for illustrative purposes only: ©iStock/Teka77
Drug name: tocilizumab (brand name Actemra)
Type of drug and what it does: Tocilizumab is an anti-inflammatory, human monoclonal antibody. It’s often used to treat rheumatoid arthritis and systemic juvenile idiopathic arthritis, a severe form of arthritis in children. The drug has the potential to block interleukin-6 (IL-6), a chemical that plays a key role in the body’s immune response and is involved in the development of many diseases. They include autoimmune diseases, prostate cancer, and multiple myeloma, which causes cancer cells to accumulate in bone marrow and crowd out healthy blood cells.
FDA approval status: emergency use authorization
Which COVID patients receive it: Per the FDA’s emergency use authorization in June 2021, tocilizumab can be used to treat hospitalized adults and pediatric patients (two years of age or older) with severe COVID-19 who are receiving systemic corticosteroids and require supplemental oxygen, non-invasive or invasive mechanical ventilation, or extracorporeal membrane oxygenation, a form of life support. Tocilizumab is not authorized for use in outpatients with COVID-19.
VA role, if any, in research on the treatment: The VA hospitals in Houston and Miami were among the nearly 70 medical sites that participated in an international double-blind study on tocilizumab. In hospitalized patients with COVID-19 pneumonia not receiving mechanical ventilation, tocilizumab reduced the likelihood of progression to mechanical ventilation or death, but it did not improve survival. In another trial that researchers from the Bronx VA participated in, use of tocilizumab did not result in significantly better clinical status or lower mortality than placebo at 28 days.
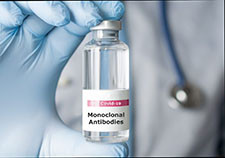
Photo for illustrative purposes only: ©Christian Storto Fotografia
Therapy name: monoclonal antibodies
Type of therapy and what they do: Monoclonal antibodies are lab-made proteins that mimic the immune system’s ability to fight off harmful pathogens, such as viruses like COVID-19. Monoclonal antibodies may block the virus that causes COVID-19 from attaching to human cells, making it more difficult for the virus to reproduce and cause harm.
FDA approval status: The FDA has issued emergency use authorization for three monoclonal antibody treatments for COVID-19: bamlanivimab plus etesevimab, casirivimab plus imdevimab, and sotrovimab.
Which COVID patients receive it: people with mild or moderate COVID-19
VA role, if any, in research on the treatment: ACTIV-3, an ongoing inpatient trial, involves about 20 VA medical centers. This trial has been testing combinations of monoclonal antibodies and antiviral drugs. VA authors contributed to papers on sotrovimab and bamlanivimab that appeared, respectively, in the journal The Lancet Infectious Diseases and in the journal Annals of Internal Medicine.

Photo courtesy of the Southern Nevada VA
Therapy name: convalescent plasma
Type of therapy and what it does: Convalescent plasma is a liquid part of human blood that contains antibodies (proteins) to certain infections, such as COVID-19. It’s believed that antibodies from convalescent plasma can directly attack the virus that causes COVID-19, as well as cells that the virus has entered, although studies have shown conflicting results on the benefits of convalescent plasma. The plasma must be typed as if someone were giving a transfusion of blood with red or white cells in it. Plasma by itself doesn’t contain red or white cells.
FDA approval status: emergency use authorization
Which COVID patients receive it: hospitalized patients early into the disease
VA role, if any, in research on the treatment: VA cooperated with the Mayo Clinic , a renowned U.S.-based medical center, on an expanded access study to evaluate convalescent plasma therapy for COVID-19. (Expanded access is a way for a patient with a life-threatening or otherwise serious condition to gain access to an investigational medical product for treatment outside of a clinical trial when no comparable or satisfactory therapies are available.) VA CURES-1 , a randomized, placebo-controlled trial, was launched to determine the benefit of convalescent plasma in hospitalized Veterans requiring supplemental oxygen. It was stopped because the researchers were unable to enroll enough participants.
--- Mike Richman
VA Research Currents archives || Sign up for VA Research updates