Office of Research & Development |
 |
Office of Research & Development |
 |


Veterans who use either lower-limb or upper-limb prosthetic devices, such as the myoelectric arm shown here, stand to benefit from work being done at the Cleveland VA to develop new materials for socket liners. (Photo courtesy of Providence VAMC)
June 11, 2020
Mike Richman
VA Research Communications
"[This] will go a long way toward improving comfort on a daily basis for amputees."
The Advanced Platform Technology Center at the Louis Stokes Cleveland VA Medical Center is highly regarded for developing innovative technologies that serve Veterans with sensory, motor, or cognitive deficits, as well as limb loss.
Advanced robotics, bionic limbs, microchips, and neural interfaces are some of the more glitzy projects that result from the ingenuity at the VA facility, which is also known as the APT Center.
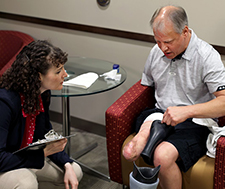
A Veteran amputee discusses his prosthetic socket liner with Courtney Shell, a research associate at the APT Center. (Photo by Jennifer Kerbo)
At the same time, scientists, engineers, and clinicians at the APT Center work on technologies that are less “sexy” on the surface but are just as important as the others. One of the ongoing projects is aimed at developing a material to better absorb and channel the sweat that can build up inside the socket liner of a prosthesis. Excess perspiration can affect the fit of a socket liner—a flexible, cushiony material that fits over the residual limb and reduces movement and chafing between the skin and the socket—and it can contribute to human tissue softening from constant water exposure, as well as infection, discomfort, and poor hygiene.
Experts at the APT Center believe that managing this issue could revolutionize the clinical implementation of socket liners. They hope the new material will provide a more stable and comfortable separation between the limb and the socket.
“People really enjoy reading about some of those other pieces of work that we do,” says Dr. Paul Marasco, a neuroscientist and principal investigator at the APT Center who is leading a developmental study on the new socket liner material. “This is probably one of the most important studies that I’m doing because it addresses a really critical problem with amputees and the VA population.”
The project is a collaborative effort involving the APT Center and the Cleveland VA prosthetics clinic, and their colleagues at the University of Chicago and Case Western Reserve University. To get the initiative off the ground, the APT Center funded the early prototype development of the socket liner through its Steven Garverick Innovation Incentive Program.

A study participant with an above-elbow amputation prepares to don her prosthetic arm. Her residual limb is covered with a smooth, pliable silicone liner to avoid irritation from the hard socket that connects the prosthetic arm to her body. (Photo by Courtney Shell/APT Center)
Conventional silicone socket liners have advanced relatively little over the years. They have a troubling tendency to accumulate sweat during use, especially for physically active amputees. Veterans have become more active in recent years due to advancements in prostheses technology, leading to a greater accumulation of perspiration. Heat and humidity can also increase moisture levels.
The new APT technology is applicable to all types of amputees—single, double, triple—but Marasco believes it can best help double and triple. He explains that single amputees can compensate for less-than-ideal socket conditions and fit, for example, by placing more weight on their sound side, thus reducing the amount of pressure or sweat that accumulates in the prosthetic socket liner.
But such compensation, Marasco notes, can lead to serious back, joint, and limb problems. “That’s going to cost severely 10, 15, 20 years down the road,” he says. “With multiple amputees, that’s a situation where the difficulties with socket fit are salient and clear right off the bat. These amputees don’t have a sound other-side limb to compensate for the poor socket fit, so they’re stuck.”
When discussing prosthetic socket moisture distribution in relation to Veterans, the focus is mostly on lower-limb amputees. Nearly all the amputees who are seen at the Cleveland VA prosthetics clinic are fitted with lower-limb prostheses, Marasco says. Diabetes is the leading cause of lower-limb amputation in the Veteran population, he notes.
“Improving water management in this critical component will fundamentally improve standard of care for a large population of upper- and lower-limb amputees,” Marasco and his team write. “A liner material which keeps this moisture away from the amputee’s skin would improve comfort and hygiene, but also the critically important fit and thus the overall performance of the prosthesis.”

VA engineering research center posts another invention: prosthetic hook mouse

Study probes user satisfaction with upper-limb prostheses

Study supports long-term benefits of non-drug therapies for pain
Marasco and his colleagues are hoping to develop a three-layer liner system made of advanced hydrated materials that eases the ability of the moisture to pass through, for use in place of the traditional water-impermeable silicone liners. The moisture becomes a problem with traditional liners by staying trapped against the amputee’s skin inside the liner.
The research team aims to address that problem by developing a system that can absorb and manage sweat possibly at a rate faster than moderate sweat production without leaking, changing size, or changing stiffness. The system is also being designed to withstand forces similar to those that would be applied in heavy use by lower-limb amputees, while still maintaining a tight seal with the skin to achieve a good fit.
“With the traditional socket liners, the moisture pools in the bottom of the liner or squelches out of the top if there is truly excessive accumulation,” says Marasco, who is also on the staff at the Cleveland Clinic Lerner Research Institute, which applies advanced research technologies, such as bionic sensory motor systems, to the needs of patients. “Amputees have to remove the liner, then pour out the moisture. Amputees sometimes wear a sock inside the liner to help absorb moisture. But that is uncomfortable and can damage skin on the residual limb due to the way they have to carry weight on the amputated bone. The skin of your shin, for example, is not nearly as tough as the skin on the soles of your feet. The weave of a sock, especially on wet skin, can cause blisters and sores.”
Marasco explains how his hydrated material system works:
“Suction socket liners are made of silicone, or vinyl polymers, which are long chains of molecules that join to make a rubbery material. We just changed how these long chains connect with each other so they make tiny channels in the silicone for the sweat to pass through. The sweat is captured in a layer of aerogel, which is another advanced material that works like a fancy sponge. The material holds sweat, but it doesn’t expand, and the water doesn’t get pushed out when the amputee puts weight on the liner.
“The trick is, to pass sweat, the silicone needs microscopic channels. However, simply having holes prevents the silicone from maintaining a proper suction seal, which is why normal silicone works so well. That’s where the water comes in. The materials we developed are hydrated, which means that water is attracted to the channels and stays inside them. The sweat can move through the liner. But it never really dries out, which explains how we have a silicone material with holes that can also maintain that critical suction seal. There’s a lot of sophisticated chemistry and microscopic structure in these materials that makes the silicone pass and store the sweat to keep the liner dry inside.”
The trial to test and develop the advanced socket liner material is multi-faceted.
So far, Marasco and his team have tested different designs of the inner wicking (absorbing, draining) layer and the middle absorption layer, measuring how much and how fast the sweat can be wicked and stored, as well as the stiffness of the layers. The researchers have also connected a sample of the inner layer to the middle layer and have tested how fast water can be wicked away and stored, and how water can be removed from the two-layer system. The team has measured size changes when the two-layer system goes from dry to wet and back to dry.

The illustration depicts a below-knee amputee removing his liner after he has taken off his prosthesis. He will dispose of any sweat in the liner, wiping it down or allowing it to air dry. To maintain good hygiene, he will also clean the liner with soap and water or alcohol at least once every few days.(Illustration by Madeline Newcomb)
In a different phase of the project, Marasco and his colleagues are examining the bacterial content of daily-use socket liners in the Cleveland VA amputee clinic. Thirty-three Veterans have participated in that part of the study. “We’re trying to get our head around the range of normal levels of bacterial load in the socket, from highest to lowest, and then to see if those measured levels correlate to the clinician’s perception of liner cleanliness,” Marasco says. “We don’t necessarily think a socket liner that’s completely devoid of bacteria is what we’re after. We want to try to build a system where the normal bacteria of your skin can live and be happy and be comfortable. But we need to know what that looks like before we can start assessing the performance of our advanced materials.”
In the end, the researchers will combine all phases of the study and test the three-layer system by recruiting 10 healthy, able-bodied people to wear a walking boot. The boot will have a sample of the new material in the heel in order to test its performance during heavy use. Some of these people will likely be Veterans. “We’ll be trying to get the material sweaty, get it used, and make sure it doesn’t fracture into pieces,” Marasco says. “We’re also going to put it on the bottom of people’s feet, let them walk on it, and then compare the bacterial load to the results of our Veteran bacterial load study.”
After the developmental project, the goal is to scale materials production up to a full-size prosthetic socket liner and test it with amputees. The scientists also need to compare bacterial growth in the advanced liner system with that of traditional liners.
“We hope the system can be commercialized soon, perhaps two to five years,” Marasco says. “It will go a long way toward improving comfort on a daily basis for amputees.”
VA Research Currents archives || Sign up for VA Research updates