Office of Research & Development |
 |

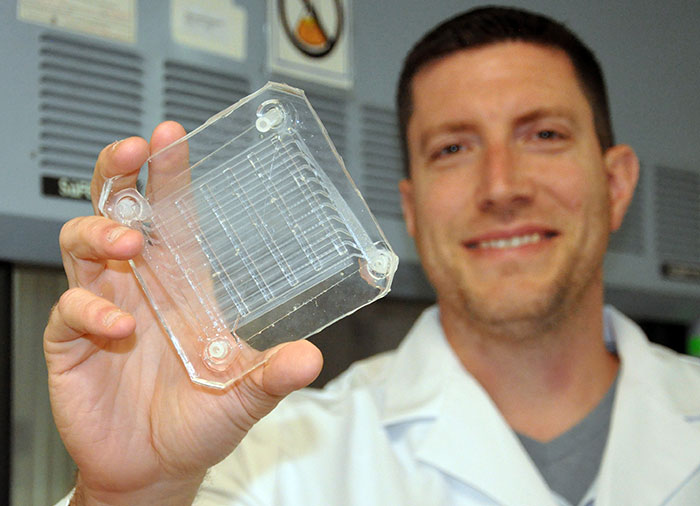
Biomedical engineer Dr. Joseph Potkay, with the VA Ann Arbor Health Care System, displays a 2D prototype of an artificial lung. A 3D version is in production. (Photo by Brian Hayes)
August 1, 2018
By Mike Richman
VA Research Communications
"We hope that these microfluidic flow paths and biocompatible coatings will be more compatible with living tissue, thereby reducing the body’s immune response and increasing the lifetime of the device."
VA scientists are working to create a 3D-printed artificial lung that they tout as having the potential to revolutionize the treatment of Veterans affected by lung disease.
One such lung disorder—chronic obstructive pulmonary disease (COPD)—is one of the most prevalent and costliest ailments in the Veteran population.
Dr. Joseph Potkay, a biomedical engineer at the VA Ann Arbor Health Care System in Michigan, is leading the VA-funded research. It calls for making a prototype of the 3D-printed artificial lung. Potkay and his team hope to build what they call the first wearable artificial lung that is compatible with living tissue and is capable of short- and long-term respiratory support.
The lung is seen initially as a temporary measure, a bridge to help patients awaiting a lung transplant or an aid for those whose lungs are healing. Future versions could have longer-term applications, the researchers say.

Potkay works with a test print of artificial capillaries that will be part of a 3D artificial lung now in production. (Photo by Brian Hayes)
Potkay says this is the first time high-resolution 3D polymer printing is being used to create microfluidic lungs with three-dimensional blood flow networks.
Microfluidic artificial lungs, a new class of artificial lungs, mimic the structure of the natural lung better than conventional artificial lungs. Tiny blood channels, some thinner than a human hair, are closer in shape and dimension to those in a person, allowing for blood flow similar to that in the human body.
The biocompatible coatings on the lung’s surface are equally important. Anytime blood comes in contact with an artificial surface, an immune response leads to hardening of the blood and clotting. Biocompatible coatings will help curtail that immune reaction.
“We hope that these microfluidic flow paths and biocompatible coatings will be more compatible with living tissue, thereby reducing the body’s immune response and increasing the lifetime of the device,” says Potkay, who is also a researcher at the University of Michigan. “The flexibility in design afforded by 3D printing gives us more freedom and thus the ease to build artificial lungs with a small size and pressure drops that are compatible for operation with the body’s natural pressures.”
For more than a decade, Potkay has been researching the advantages of microfabrication, the recreation of tiny structures, to build artificial lungs that have highly efficient gas exchange and blood paths similar to those in a human lung. Gas exchange is the amount of oxygen or carbon dioxide (CO2) that is transferred into or out of blood in the artificial lung.
“However, microfabrication is mainly a two-dimensional construction technology,” he says. “With a 2D design, you stack many single 2D layers together. That has limited the ease of creating devices that are large enough for human use. You have less freedom in how you design the blood channels. 3D printing these devices may be a solution to these problems. We can be much more precise and efficient with how the blood flow path is laid out in three dimensions.”

Potkay’s artificial lung model relies on microfabrication, the recreation of tiny structures, to achieve highly efficient gas exchange and blood paths similar to those in a human lung. (Photo by Brian Hayes)
Potkay’s team is working with Old World Labs, a company in Hampton, Virginia, that specializes in high-resolution 3D printing. The firm should be able to produce a small-scale functional prototype sometime in the coming months, he says. The prototype will be about a half-inch cube in size, and the 3D-printed human-scale lung should occupy no more than a six-inch cube space, he notes.
Potkay envisions the human 3D device fitting in a backpack or a small butt pack, with potential use of more than a week. After more development, he expects longer-term use will be possible.
He says it’s impossible to gauge how many years away the 3D-printed lung is from implantation, noting that it must first be tested on animals and people. “We’ll see how well it does in terms of lifetime,” he says. “To be implantable, it needs to be able to operate for months without being swapped out.”
Heart-lung machines that contain artificial lungs have long been in use to rehabilitate lung disease patients. But these machines are bulky pieces of equipment in which all components are mounted on a wheeled pole. Some people call these portable or ambulatory lungs, but in Potkay’s view they are not truly portable.
These machines also require pure compressed oxygen stored in heavy cylinders. However, major advances in gas exchange, compatibility with living tissue, and portability are needed for artificial lungs to fully realize their potential. The device must also maintain appropriate blood pressure, decrease injury to blood cells, and minimize clotting and immune response.
Microfluidic artificial lungs use a fraction of the volume of blood of current commercial devices.
In their research, Potkay and his colleagues are focusing on patients with a buildup of CO2 in the blood, an occurrence that applies to many Veterans suffering from end-stage chronic obstructive pulmonary disease. End-stage COPD is marked by severe shortness of breath, chronic coughing, lung infections, or respiratory failure. It can lead to sudden cardiac death. Excess CO2 must be removed from the lungs to stop it from reaching unhealthy levels.
COPD affects 5 percent of American adults and 16 percent of the Veteran population. Most people with COPD have emphysema, in which the air sacs of the lung are damaged and enlarged, and chronic bronchitis, a long-lasting cough caused by chronic inflammation of the bronchial tubes. The disease is characterized by an airflow limitation that is often linked to an abnormal response of the lungs to noxious particles or gases, such as those in cigarette smoke.

Research roundup: E-cigs aren't safe

VA works to raise awareness for lung cancer screening in Veterans
Some returning Vets are not breathing easy: Could war-zone dust mites be part of the problem?

When non-adherence to guidelines is a good thing: Study on COPD yields surprising results
Exposure to burn pits, sand, diesel exhaust, and chemicals are some of the most commonly cited factors that lead to lung problems for active-duty military. About 20 percent of patients with severe traumatic brain injury also have acute lung injury.
In 2011, Potkay unveiled a prototype of a 2D-printed artificial lung that used traditional microfabrication techniques. It was a collaborative effort between Case Western Reserve University in Cleveland and the Advanced Platform Technology Center at the Louis Stokes Cleveland VA Medical Center. Potkay was affiliated with that VA facility at the time.
The prototype was unique in how it copied nature. Because of its intricate silicon tubing and ultra-thin gas diffusion membrane, the device was efficient enough to use air as the ventilating gas—as opposed to pure oxygen stored in a tank. It thus created new possibilities for portability and possibly implantation.
The 3D-printed lung will provide the same basic advantages, Potkay says.
“But with the freedom afforded by being able to design the device in three dimensions instead of two, 3D printing should result in artificial lungs with a smaller overall footprint and with increased efficiency,” he says. “Thus, portability and performance will potentially improve using 3D printing.”
The 2D project is ongoing in Potkay’s lab at VA Ann Arbor. He’s currently testing the device in rabbits and is pursuing the next stage of funding to scale the 2D lung up to sizes that apply to human use.
Why continue with the 2D project if the 3D lung appears to be more adaptable to the goal of creating a microfluidic artificial lung?
“Although the 3D artificial lung is more promising, it is earlier in development and still not guaranteed to work,” Potkay says. “We’re further along in developing the 2D device, and we have plans to work around the challenges with that device.”
Lab testing of the 2D artificial lung has provided a glimpse of what Potkay and his colleagues are capable of achieving in a 3D format.
In tests with animal blood using traditional microfabrication techniques, the small-scale artificial lungs achieved the highest gas efficiency exchange of any artificial lung to date, according to Potkay. He expects the “excellent performance” to translate to the 3D lung.
In addition, he says, the initial expected lifetime of the 2D lung of more than a week—identical to the 3D lung—“significantly improved” because of the biocompatible surface coatings that mimic the cell wall. He expects those findings to also apply to the 3D device.
In terms of lifetime, “We believe the 3D-printed device should be better than the 2D version, but we don’t have proof yet,” he says.
When the study ends next year, Potkay and his colleagues hope to test a prototype of their high-resolution 3D-printed artificial lung in a large animal model, most likely sheep.
In addition to COPD, Potkay says the 3D lung could be used as a temporary measure for people with lung diseases such as acute respiratory distress syndrome. That condition is a leakage of fluid into the lungs that makes breathing difficult or impossible.
“It will depend largely on the needs of the patient,” he says. “The removal of CO2 in the blood is the first Veteran application we’re aiming for because it’s the simplest in terms of patient use, the required components, and the size of the device. CO2 removal is a critical need for many Veterans with COPD.”
VA Research Currents archives || Sign up for VA Research updates