Office of Research & Development |
 |
Office of Research & Development |
 |


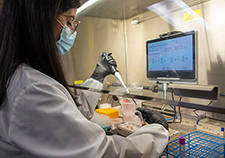
Dr. Kristina Crothers of VA Puget Sound is leading the collaboratory’s investigation into steroids, which provide relief for inflamed areas of the body. Steroids are one of the three classes of drugs the COVID-19 collaboratory is examining. (Photo by Chris Pacheco)
October 16, 2020
By Mike Richman
VA Research Communications
"We want to work systematically to support analyses that have the most promise to be useful and to complement efforts of clinical trials."
For decades, VA has been using electronic health record data to explore patterns of care and the effectiveness of treatments. But the COVID-19 era has highlighted the challenges of getting such analyses right. To do so, one must have a deep understanding of the intricacies of VA data, including how reliable they are, the differences in patients who get certain treatments, and how COVID-19 therapies have changed over time.
The disease has created a need and an opportunity for VA to improve the quality of the analyses using electronic health record (EHR) data by drawing on the collective knowledge of researchers with decades of experience conducting observational studies.
That’s the thinking behind VA’s COVID Observational Research Collaboratory. The initiative brings together VA experts to analyze the use and effects of drugs with clinical partners interested in the safety and effectiveness of COVID-19 therapies. VA’s Health Services Research and Development Service (HSR&D), Clinical Science Research and Development Service, and Cooperative Studies Program established the collaboratory soon after the pandemic took hold earlier this year.

VA center training the next generation of researchers in blood clots and inflammation

AI to Maximize Treatment for Veterans with Head and Neck Cancer

VA researcher works to improve antibiotic prescribing for Veterans
VA’s Million Veteran Program played crucial role in nation’s response to COVID-19 pandemic
“We want to work systematically to support analyses that have the most promise to be useful and to complement efforts of clinical trials,” says HSR&D director Dr. David Atkins, the head of the collaboratory. “We want to reuse what we learn from each study to improve the quality of the data and the design of observational treatment studies. The feeling is there may not be only one way to do analysis, but there certainly are problems to avoid and ways to probably do it better. The more we can communicate and learn from each analysis we do, the hope is each one will get better and better and more efficient.”
The VA collaboratory was built on the model of similar programs set up by the U.S. National Institutes of Health (NIH) to try to improve coordination across projects and data methods. NIH’s National Center for Advancing Translational Sciences and the NIH Health Care Systems Research Collaboratory, for example, bring together research teams with complementary skills, experience, and knowledge to accelerate learning in specific areas, such as non-opioid therapies for chronic pain.
Similarly, VA is trying to unite scientific experts who have been working on similar questions to expand its understanding of COVID-19 treatments in a Veteran population. The goal is to then improve approaches to using VA data by getting input from a range of experts in pharmaco-epidemiology—the long-term study of medications—and data methods.
The collaboratory has created two work groups: The prioritization work group is identifying important questions related to COVID-19 therapies, in collaboration with similar efforts at the U.S. Food and Drug Administration (FDA), that could be investigated using EHR data. The other work group is addressing ways to improve the underlying the data and methods used to address these questions. These efforts build on work initiated by Dr. Amy Justice, a clinical epidemiologist at the VA Connecticut Healthcare System, and they operate alongside analytic efforts involving VA, the U.S. Food and Drug Administration (FDA), and the U.S. Department of Energy.
The collaboratory’s goals have changed over time. When the pandemic first broke, there were no effective treatments and “people were kind of grasping for straws,” Atkins explains. The thought was to use observational data to see what clinicians were trying and whether something seemed to be working, with the aim of testing it in a clinical trial, he notes.
Now that effective therapies have surfaced through clinical trials, and many other trials of other drugs are underway, the research community is less interested in trying to identify new drugs for studies. “We’re looking at drugs that have been tested in trials like [the antiviral drug] remdesivir,” Atkins says, “and are asking whether we can use the observational data to fill in some of the unanswered questions.”
Remdesivir (trade name Veklury) is in one of the three classes of drugs the collaboratory is examining. A randomized controlled trial published in May found that the drug shortened the recovery time for hospitalized COVID-19 patients with lower respiratory tract ailments. In response, the FDA issued an emergency use authorization to allow rapid access to remdesivir during the COVID-19 pandemic.
Dr. Michael Ohl, an infectious disease specialist at the Iowa City VA Health Care System, is leading a study for the collaboratory that aims to understand how remdesivir is being used to care for COVID-19 patients in VA hospitals.
“Our research will inform efforts to ensure efficient distribution of this new medication,” Ohl says. “We also intend to address questions about the effectiveness of remdesivir that could not be answered in clinical trials, such as which patients benefit most from the medication in routine clinical practice and the effectiveness of remdesivir in combination with other promising COVID-19 therapies.”
The collaboratory is also examining anticoagulants (blood thinners), which eliminate or reduce the risk of blood clots. Preventing blood clots is of great interest to VA because severe COVID-19 features an inflammatory response that is marked by cardio and blood vessel complications, with risks of heart attack, stroke, and blood clots in the veins. There is little data to determine whether blood thinners and what type of blood thinner can effectively prevent these health problems, Atkins says. The FDA prioritized this question in its Coronavirus Treatment Accelerator Program.
The research community has recognized that thrombosis, which happens when blood clots block blood vessels, is a big part of the pathology of COVID-19, especially extreme cases. The collaboratory’s initial analysis is focused on hospitalized patients who get prophylactic anticoagulation, which is often administered to prevent deep venous thrombosis in the legs.
But no definitive studies have shown that prophylactic anticoagulation can reduce the risk of death from thrombosis. In addition, it’s unknown whether anticoagulants can prevent clotting associated with COVID, or what type of anticoagulant, dose, or timing would be needed. There are three general classes of anticoagulants: those usually given in the hospital for short-term use; a long-term pill for people prone to clots or with artificial heart valves; and newer drugs that are simpler and act through different mechanisms.
“We hope to learn the role of prophylactic anticoagulation to potentially reduce the risk of death from thrombosis among hospitalized Veterans infected with COVID-19 who are not on anticoagulation before admission,” says Dr. Christopher Rentsch, a pharmaco-epidemiologist at the VA Connecticut Healthcare System. “We will also examine, separately, the Veterans who are infected with COVID-19 and are on pre-existing therapeutic levels of anticoagulation for non-COVID health conditions like atrial fibrillation.”
The VA collaboratory is also focusing on corticosteroids, which provide relief for inflamed areas of the body. A British study showed that in hospitalized COVID-19 patients, the steroid dexamethasone (trade name Decadron) resulted in lower 28-day death rates among those receiving invasive mechanical ventilation or oxygen at randomization, but not among people with no respiratory support.
Dr. Kristina Crothers, the section chief of pulmonary, critical care, and sleep medicine at the VA Puget Sound Health Care System in Washington State, is leading the investigation into steroids. While emerging data suggest a benefit of steroids for COVID-19 patients, it remains unclear which patients should receive them, as well as other factors related to the therapy, she says.
“This includes when in the course of illness and which type of corticosteroid, dose, and duration of therapy should be used,” she says. “We also don’t understand how being on steroids before illness might impact the use and response to steroids when someone gets acutely ill with COVID-19.”
The collaboratory, Crothers notes, is using EHR data to conduct a retrospective cohort study to help address these questions.
“We hope to learn whether steroids decrease the risk of worse outcomes in hospitalized Veterans with COVID-19, particularly risk of mechanical ventilation and death, as well as evidence of other end-organ failure,” she says. “We will also consider dose and type of steroid used. We will additionally compare rates of complications that can be associated with steroids in patients, such as delirium, secondary infections, and elevated blood glucose levels.”
Through the collaboratory, VA has a “unique opportunity” to examine questions about COVID-19 drugs due to its population size and the quality of its EHR data, Atkins notes.
“There was a danger that multiple VA teams would be competing with each other to do analyses as quickly as possible,” he says. “Especially in an era of preprints, there is a concern that the first VA study to get attention wouldn’t be the best VA study. We’re trying to set up a coordinating center not only to review a research team’s study protocol, but also so the analysis and manuscripts would get vetted before being submitted. That’s one of our top priorities as we move forward with the collaboratory.”
VA Research Currents archives || Sign up for VA Research updates