Office of Research & Development |
 |
Office of Research & Development |
 |

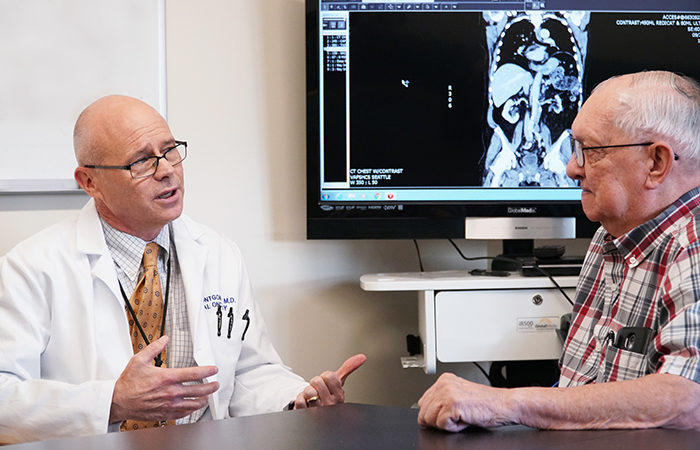
Dr. Bruce Montgomery meets with Navy Veteran Allen Petchnick, whose prostate cancer has been effectively treated to date with targeted therapy. (Photo by Christopher Pacheco)
November 13, 2019
By Mike Richman
VA Research Communications
While in treatment for an aggressive form of prostate cancer at the VA Puget Sound Health Care System in Seattle, Navy Veteran Allen Petchnick faced a daunting situation. His PSA blood test, the main screening tool for cancer of the prostate, had risen to 13, which for him was dangerously high. Plus, his cancer had spread to other parts of his body.
“He was looking at very tough outcomes,” says Dr. Bruce Montgomery, an oncologist at VA Puget Sound. “He was passing out because his tumor had metastasized to lymph nodes in his neck, which was pressing against one of his arteries.”
Montgomery led a medical team that performed next-generation sequencing, an innovative way to sequence the human genome at high speed and low cost, on tissue in Petchnick’s lymph nodes. They spotted mismatch repair (MMR) deficient cells, which usually have many genetic mutations—the changing of the structure of a gene—that may lead to cancer. Knowing if a tumor is MMR-deficient may help clinicians plan treatment or predict how the tumor will respond to treatment. This is an example of precision oncology.
"Those patient stories made it very clear to us...why this is so urgent and how transformational the opportunity to partner with VA can be."
Petchnick received immunotherapy, a form of precision oncology in which organisms in the body’s immune system are used to fight cancer. Now age 79, he’s been on immunotherapy drugs for nearly two years, during which time his PSA (prostate specific antigen) level has become undetectable and the tumor continues to shrink, Montgomery notes.
“He went from basically being unable to get out of a chair to going shopping with his granddaughter in just one cycle of therapy,” Montgomery says. “He may be cured. But we’ll only know that when we stop his therapy, which is likely to happen soon. Right now, he’s very close to a complete response after looking like he was going to be in very difficult straits.”
Petchnick is one of several major success stories that have surfaced from an advanced level of medical care made possible by a partnership between VA and the Prostate Cancer Foundation (PCF), a philanthropic group that funds research to prevent and cure prostate cancer. The partnership is centered on speeding the development of treatment and cures for Veterans with aggressive—or metastatic—prostate cancer through precision oncology.

VA researchers using AI to decide best treatment for rectal cancer

VA center training the next generation of researchers in blood clots and inflammation

AI to Maximize Treatment for Veterans with Head and Neck Cancer

VA investigator brings diversity into autoimmune disease research
The procedure involves the molecular profiling of tumors to identify targetable genetic mutations through means such as immunotherapy, chemotherapy, and targeted therapy, all of which are used to kill aggressive cancers that have spread in the body. Targeted therapy, which works by targeting the genes, proteins, or tissue that contribute to cancer growth and survival, can be immunotherapy or chemotherapy, as long as it’s being used because of a specific marker or target that makes it more likely to work.
Precision oncology is fast developing and has entered the mainstream of clinical practice, with application to a myriad of cancers. Each cancer patient may have different mutations in play, and researchers are learning how to leverage this genetic information to improve outcomes.
VA and PCF signed the agreement in 2016 and put it into action early this year. It comes at a time when more than 16,000 Veterans are diagnosed each year with prostate cancer, making it the most common solid tumor cancer among Veterans.
“Our goal is to increase our scientific understanding of prostate cancer among Veterans and to kick-start the development of precision medicine treatments for them, as well as the general population,” Dr. Jonathan Simons, president and CEO of the Prostate Cancer Foundation, said in a video produced by PCF. “This agreement will open new doors for the research community to work with Veterans facing a life-threatening disease and ultimately reduce the disease burden on America’s Veterans.”
Rebecca Levine, national director of PCF’s Veteran health initiative, says the foundation felt compelled to partner with VA also because some of its board members are Veterans who had life-extending results after participating in prostate cancer trials. “Those patient stories made it very clear to us in a personal way why this is so urgent and how transformational the opportunity to partner with VA can be,” she says, “given what PCF brings to the table in science and what VA brings to the table with its large patient population.”
In Bruce Montgomery’s view, PCF decided that investing its research dollars in a national integrated health care system like VA would provide the most impactful return.
“There was obvious interest on their part in precision oncology,” he says. “They also saw VA’s resources with regard to integrated data and clinical elements as something that could in the big picture and over the long term provide critical insights into how we might reach men who have advanced prostate cancer and give them the best access to health care. The whole idea behind this effort was to stand up an integrated precision oncology system in VA and show that if we can do this in the biggest health care system in the U.S., then the optimal efficiency and outcomes can be extended outside of VA and provide better results for everybody.”
Prostate cancer, the second-leading cause of cancer deaths among men, is most common in men age 65 and older. The disease is usually found in its early stages, typically due to PSA screenings, and often grows slowly. It may take many years for a tumor to become large enough to be detectable and even longer to spread beyond the prostate, the walnut-size gland that sits just outside the rectum and bladder and forms part of the male reproductive system. Most men who have the cancer live with it for decades without symptoms and die of other causes even without early surgery. But a subset of men quickly develop more aggressive prostate cancer—the focus of the VA-PCF effort.
Currently, nearly 500,000 living Veterans have been diagnosed with prostate cancer. Of those, an estimated 3% have metastatic prostate cancer.
PCF donated $50 million to VA in the five-year partnership. It calls for increasing the number of VA facilities that are doing precision oncology and prostate cancer clinical trials, raising the number of VA researchers applying to PCF for funding, and getting more Veterans enrolled in studies. About half of the funding is aimed at building a network of VA sites that are doing precision oncology. The network now includes 10 sites: Washington; Philadelphia; Seattle; Los Angeles; Chicago; Ann Arbor, Michigan; Durham, North Carolina; Tampa, Florida; Bay Pines, Florida; and New York City, in Manhattan and the Bronx. The goal is to eventually have at least one network site in each of the 21 VISNs (Veteran Integrated Services Networks) into which the VA health care system is divided.
The network has launched a series of multisite clinical trials that aim to sequence as many Veterans as possible so they can have access to precision oncology. VA’s Office of Research and Development and the Prostate Cancer Foundation are supporting these trials.
“We are excited to be one of the 10 VA sites in the network,” says Dr. Kyong-Mi Chang, associate chief of staff at the Corporal Michael J. Crescenz VA Medical Center in Philadelphia. “These sites provide resources needed to improve the care of our Veterans together as a network, and to enhance access to state-of-the-art clinical trials for Veterans using precision oncology and genomic medicine.”
The other half of the funding is going to scientists for special projects on prostate cancer. Case in point: Dr. Jeffrey Jones, the chief of urology at the Michael R. DeBakey VA Medical Center in Houston, is studying the impact of Agent Orange, the Vietnam War-era herbicide that the U.S. used to destroy forested areas, on patients with prostate cancer, as well as disparities among Veterans of African ancestry who have prostate cancer. African-American men are 60% more likely to develop prostate cancer, compared with any other race or ethnicity, and 2.4 times more likely to die from the disease.
“For many different reasons, African-American men are at higher risk for having what we consider to be lethal prostate cancer, not the kind of prostate cancer that people live with,” Montgomery says. “We think genetics plays a role. Why else would they be at such risk? Although nobody has been able to pinpoint a single gene that is causing lethal prostate cancer in African-American men, VA investigators are working to define causes. Other reasons could be things like access to care, but that’s far less of an issue in VA because it’s an equal-access system. Access to insurance and access to care in the big wide world is more difficult for a number of ethnic groups, including African-Americans.”
In turn, VA is making patient data on prostate cancer cases available to approved VA researchers, with patients’ prior consent, from sources such as VA’s Million Veteran Program (MVP), which aims to enroll a million Veterans to understand how genes affect health and illnesses. About 150 researchers affiliated with VA or partnering academic institutions are working on projects through the VA-PCF partnership.
Montgomery is now leading a pilot project looking at normal DNA from the more than 800,000 Veterans who are enrolled in MVP. He and other clinicians are sequencing a specific set of genes, including BRCA1 and BRCA2. Both genes are known to increase the risk of such cancers as breast, ovarian, and prostate (see sidebar).
“So we actually can look and tell that 300 men in MVP who have metastatic prostate cancer have these alterations,” Montgomery says. “We’re just launching a pilot project where we’re reaching back out to the men who participated in MVP. We’re telling them that we may have found a genetic result that could benefit them in their care and are asking if they’d like to participate in genetic testing. We offer them clinical retesting because the MVP sequencing isn’t a clinical-level sequencing assay. We expect every one of [the retests] will agree with the original MVP sequencing. They then will have access to alternative approaches that can give them better outcomes.”
One of the leading elements of the VA-PCF collaboration, precision oncology, is influenced mainly by advances in sequencing technology. The technology has advanced to the point that it has allowed the human genome—all of the genetic information in a person—to be sequenced in less than a day for about $1,000. This is a fraction of the time and expense involved only a few years ago. Sequencing allows clinicians to extract data from tumors on an individual basis and to learn about the genetic changes within the mutations that are driving a person’s cancer. Consequently, doctors can identify the right drugs based on a patient’s mutation and decide whether chemotherapy, immunotherapy, or targeted therapy would be appropriate.
The normal sequencing procedure of all DNA in a patient is usually done 5 to 50 times. In the next-generation sequencing performed in the VA-PCF network, scientists are sequencing specific regions an average of 500 to 1,000 times, depending on where the gene is located, Montgomery says. The greater frequency results in more accurate readings.
Dr. Matthew Rettig is an oncologist at the VA Greater Los Angeles Health Care System, which is part of the VA-PCF network. He explains that not all of the 19,000 genes in the human genome are sequenced as part of the process. Several hundred genes are selected because of the frequency with which they mutate in cancers in general, he says.
“One wants multiple reads on a region,” Rettig says. “That’s particularly important in cancer because very often the tissue we’re using as a source of tumor DNA is contaminated with normal DNA, which is often the dominant form of DNA. So when you do a prostate biopsy, perhaps only 20% of the specimen is the tumor. Imagine if you had a single read of a region of DNA. It was only covered one time in the sequencing process, and 90% of the DNA is non-tumor DNA. The greatest likelihood is that you would get a sequence that was non-tumor. So it has to be sequenced multiple times to be able to capture the cancer sequence.”
Each site in the network is focused on finding molecular drivers of prostate cancer by performing next-generation sequencing on the tumors of Veterans with metastatic prostate cancer. The patients then get access to optimal therapy through biomarker-driven clinical trials, use of therapies approved by the U.S. Food and Drug Administration (FDA) with “exceptional responses,” and off-label use of FDA-approved drugs.
“The main focus of these sites is to really pressure-test the system in VA so we can get all of the bugs out,” Montgomery says, “so when we have lessons learned about how best to do this the process will be as efficient and effective as possible across VA.”
The sequencing is not done at the VA sites in the network, but at laboratories at VA-PCF partnership facilities: the University of Michigan, the University of Washington, and Memorial Sloan Kettering Cancer Center in New York City, as well as through the VA National Precision Oncology Program (NPOP). Using genomic medicine, NPOP aims to bring precision cancer treatment to Veterans. (The NPOP sequencing is done through a commercial vendor. But NPOP coordinates who participates and the sites where the sequencing takes place and tracks the results for use in therapy.) The findings at these labs can be used for clinical care because they are certified under the Clinical Laboratory Improvement Amendments of 1988 (CLIA), which sets guidelines for laboratory testing to ensure the accuracy, reliability, and timeliness of patient results.
“The staff at these labs have done a lot of the sequencing and have reported critical findings on prostate cancer that have appeared in high-profile journals,” Rettig says. “Identification of the relatively high frequency of hereditary cancer syndromes, for example, came out of the sequencing lab at the University of Washington. “The story with CDK-12 came out of the academic sequencing lab at the University of Michigan.” The CDK-12 gene is known to be altered in cases of prostate cancer, among other types of cancer.
As Rettig sees it, the VA-PCF partnership is making available an “incredible amount of information that we’re now able to mine” in efforts to treat and cure prostate cancer.
“This is going to impact prostate cancer research throughout the United States and globally,” he says. “You wait and see. It’s going to be unbelievable. What we have at our fingertips given the number of patients, the clinical follow-up, the fact that the patients stay within the VA system … that isn’t true in the private sector. Patients bounce around. Veterans stay in the VA system overwhelmingly. We know what’s happening to them. We know how they’re being treated. We’re going to make so many important discoveries as a consequence of this program.”

Dr. Bruce Montgomery is an oncologist at the VA Puget Sound Healthcare System. (Photo by Christopher Pacheco)
Dr. Bruce Montgomery of VA Puget Sound and Dr. Matthew Rettig of VA Greater Los Angeles have long been on the front lines of researching the molecular drivers of prostate cancer.
Less than a decade ago, the two oncologists contributed to groundbreaking research that brought the medical community closer to knowing the correct drugs and therapies for targeting tumors in about 30% of patients with aggressive prostate cancer.
The Stand Up to Cancer foundation, the American Association for Cancer Research, and the Prostate Cancer Foundation (PCF) funded the initiative. More than 1,000 men with aggressive prostate cancer underwent metastasis biopsies, in which deep sequencing was performed on soft tissue from their lymph nodes or liver, or from the bone. Sequencing metastatic tissue late in the course of the disease had never been done before in prostate cancer research, Montgomery says.
Currently, metastasis biopsy programs are in place at about half of the 10 VA sites in the VA-PCF partnership (see main story). The rest will eventually reach that stage. But other sources of tumor DNA aren’t being excluded in the biopsies, including tissue from the prostate and tumor DNA that circulates in the blood.
“In the last five years, metastasis biopsies have been done much more often, partly because of what studies like this one revealed,” Montgomery says. “Metastatic lesions have obviously acquired the ability to metastasize or spread from the primary site and have developed resistance to androgen deprivation therapy, which is often used to stop metastatic cancer cells from spreading. Primary lesions have not developed that resistance. The genetic alterations found in those cells that have passed the test of fitness to survive are more likely to be relevant drivers.”
Previously, Montgomery explains, most of the DNA sequencing on men with aggressive prostate cancer was done on what are called primary specimens—such tissue as prostatectomy or prostate needle biopsies—that reflect when the men were first diagnosed with metastatic cancer. That tissue could be at least 10 years old. “What’s happening in the tumor when they were diagnosed is not necessarily what’s happening to them now and what the primary drivers of the biology of the cancer are for that patient today,” he says.
In the metastasis biopsies, the researchers found critical details about genetic alterations that were once thought to be rare in aggressive prostate cancer. They learned that mutations of the BRCA1 and BRCA2 genes, both of which are prevalent in women with breast cancer and ovarian cancer, are much more common in men with prostate cancer than originally thought. They also found in a small percentage of the men something called mismatch repair deficiency, which is considered common in patients with colon cancer and other malignancies. The researchers also identified CDK12 as a frequent mutation in prostate cancer. CDK12 can cause a highly mutated genome due to deficient DNA repair in tumors.
“If you add all of this up, we’re in the range of about 30% of men with advanced prostate cancer who have alterations that can be targeted today because we have drugs that are FDA [U.S. Food and Drug Administration]-approved to target BRCA for breast cancer and ovarian cancer patients,” Montgomery says. “We have immunotherapy that’s FDA-approved for mismatch repair deficiency, and we have very exciting preliminary data that immunotherapy could work on CDK12-altered tumors. That basically means almost a third of men with advanced prostate cancer have something that can be targeted. The big idea is that the alterations are there. We just need to find them.”
One of the most commonly mutated genes across all cancers, P53, was included in the sequencing. However, there are no drugs or therapies that can target the P53 mutation. “As you can imagine, this is an area of great interest to the research and pharmaceutical communities,” Rettig says.
Rettig cautions that the scientific community thinks it knows how to target such mutations as BRCA1 and BRCA2 for prostate cancer therapy. The results from other types of cancer don’t always translate to prostate cancer, he says, noting that researchers are carrying out clinical trials in the VA-PCF partnership to test the therapies that would apply to the 30% group. These trials fall under a large umbrella study called PATCH (Prostate Cancer Analysis for Therapy Choice), which is funded by both VA and the Prostate Cancer Foundation. The thinking is that each possible mutation in a patient with prostate cancer would involve a different trial.
“We want to have little different baskets for different patients under one big study that covers all of the baskets,” Rettig says. “There may be a study for mismatch repair deficiency and for CDK12, another study for the BRCA mutations, and another study for P53 mutations, etc. We’re in the process of filling out the other clinical trials that would fall under this PATCH umbrella. Dr. Montgomery and I are trying to get as many ideas as we can on genetic mutations from other investigators in the VA network that would be appropriate to target with treatments, so we can have the most robust clinical trial possible.”
In Montgomery’s opinion: “One of the big areas of controversy in precision oncology is whether a mutation in one tumor means the same thing in another tumor. The short answer is that some of them do and some of them don’t. BRCA, for example, has been seen essentially across all of the malignancies in which we find these BRCA alterations. That means breast, ovarian, pancreatic, and prostate cancer. If you have a small frequency of BRCA alterations in colon cancer, that probably doesn’t mean the same thing. So the drugs that target that biology are very likely to have significant impact on outcome in BRCA-related cancers, such as prostate cancer.”
What about the other 70% of men who have metastatic prostate cancer?
“The other 70% do not have alterations that as of today, we can say, `Okay, you have the P53 alteration, and we can treat you differently as a result,” Montgomery says. “As an example, P53 is the most common alteration in human cancers of any kind, so finding drugs that work effectively in P53-altered tumors would have a significant impact. In addition to the VA-PCF partnership, the greater prostate cancer community is trying to find answers to how to effectively target these and other alterations. But there’s a huge amount of work still yet to do in trying to use these biomarkers to help to guide therapy. That’s where our energy will be going in the future—finding an answer for that subset of men who don’t have a targetable alteration.”
--- Mike Richman
VA Research Currents archives || Sign up for VA Research updates