Office of Research & Development |
 |

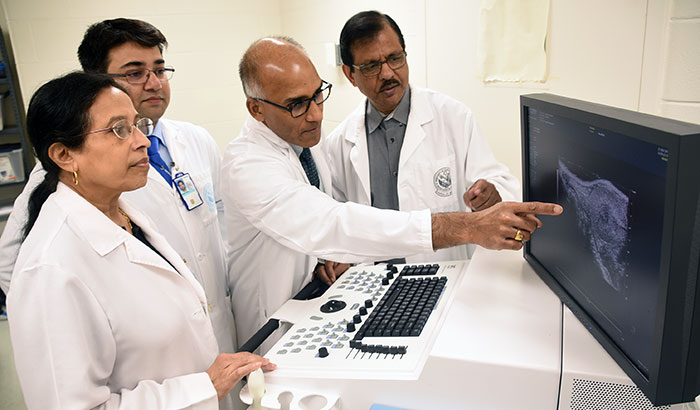 Examining a pancreatic cancer image are (from left) Drs. Snigdha Banerjee, Arnab Ghosh, Suman Kambhampati, and Sushanta Banerjee. (Photo by Jeff Gates)
Examining a pancreatic cancer image are (from left) Drs. Snigdha Banerjee, Arnab Ghosh, Suman Kambhampati, and Sushanta Banerjee. (Photo by Jeff Gates)
June 10, 2019
By Mitch Mirkin
VA Research Communications
"It's one of the most dreaded diagnoses that we can give to a patient and their family, just given the nature of this cancer and its natural history."
Pancreatic cancer is among the most devastating diagnoses anyone can receive. Only 20% of patients make it past a year, and only 9% can expect to live beyond five years. Those rates are up from a few years ago, in part due to more awareness and better screening, and wider use of aggressive combination therapies. But researchers still have a long road ahead.
The best drug currently available to treat the disease, gemcitabine, offers some benefit, but most pancreatic tumors become resistant to it early on. The drug quickly loses its punch against cancer cells.
That’s where Drs. Sushanta and Snigdha Banerjee, a husband and wife team, see an opportunity. Their lab in the Cancer Research Unit at the Kansas City (Missouri) VA Medical Center is intent on figuring out how to make gemcitabine potent over months, instead of just weeks. The group is also partnering with chemical engineers to learn how to deliver another tumor-squashing drug, zoledronic acid, directly to cancer cells via a nanoparticle. That way, it pummels those cells without hurting other tissues.
Both approaches, and especially the latter one, offer hope for the future, says Dr. Suman Kambhampati, an oncologist at the Kansas City VA who has collaborated with the Banerjees on several papers. While he doesn’t treat a lot of Veterans with pancreatic cancer—he says his VA hospital, on average, will see 5 to 10 cases a year, which is a small number compared with lung or colon cancer—they account for some of his most trying work as a doctor.
“It’s one of the most dreaded diagnoses that we can give to a patient and their family, just given the nature of this cancer and its natural history,” says Kambhampati, who has been a doctor with VA since 1996.

Male breast cancer: A rare disease, on the rise

Chemo without the side effects: Scientists look to gold, toad skin for answers
Change in cell traffic pattern could signal chemotherapy response

Fear of malpractice claims not a reason to screen for esophageal cancer
To lay the groundwork for a clinical breakthrough, the Banerjee group has identified key molecular culprits in pancreatic cancer. The gang leader is a protein called CYR61.
Importantly, the protein appears to drive three biochemical processes that make pancreatic cancer tough to treat—and that thwart gemcitabine, in particular.
Sushanta says the main question for the lab has been, “If we block CYR61, can we block all three [processes]?”
One process has to do with cancer stem cells. There is a subset of these cells, mesenchymal cells, whose population explodes early on in pancreatic cancer—thanks in part to CYR61. This pushes the tumor to grow and spread.
The second has to do with how gemcitabine gets activated in the body. Certain enzyme reactions have to take place, or the drug remains inert. “We found that CYR61 plays a vital role in blocking gemcitabine activation,” he says. “[When activation is blocked], you can give a high dose of the drug but it doesn’t work, because it’s mostly in an inactive form.”
The third has to do with the physical nature of pancreatic tumors. These masses of cancer cells form a thick fibrous shell, like scar tissue, that acts like a coat of armor to stop drugs from penetrating. The process is known as desmoplasia. “CYR61 promotes this biological barrier,” says Sushanta.
Experiments in their lab, say the Banerjees, have shown clearly that CYR61 is a key player in all three of these pancreatic-cancer hallmarks.
The team uses genetically engineered mice that carry two mutations, in genes known as KRAS and p53. KRAS and p53 mutations are common to several cancers, but the specific changes engineered in these rodents lead to pancreatic cancer. The mice develop the disease within three months of birth. Given the rapid lifespan of the mouse, that is the equivalent of a human in his mid-20s.
Most pancreatic cancer patients have these same mutations. Rather than being inherited from parents, they are acquired mutations triggered by ongoing inflammation in the pancreas. The inflammation could result from lifestyle factors like tobacco and alcohol use, and from conditions such as obesity and diabetes. Certain other toxic exposures—such as from farm chemicals—may play a role as well, suggests some research.
“These [mutations] are the results of chronic inflammation within the cellular milieu of the pancreas,” says Kambhampati.
Knocking down the levels of CYR61, in theory, could make pancreatic tumors far more vulnerable to gemcitabine. Since CYR61 is absent in the normal pancreas, and appears only when the KRAS and p53 mutations work together to exert their sinister effect, the Banerjees are not worried about possible side effects from totally suppressing the protein. They point out it serves no healthy purpose in the body.
How exactly to shut down CYR61 remains to be worked out in further experiments. The researchers have to figure out which signaling pathway to disrupt, and with which molecule. In any event, human trials of such an approach are at least a few years off.
Meanwhile, Snigdha is partnering with a team 600 miles away at North Dakota State University that has expertise in nanotechnology. This effort revolves around another drug, zoledronic acid, that mainly boosts bone health—including in cancer patients with bone-related side effects from chemotherapy.
As it turns out, zoledronic acid dials down the expression of CYR61—the pesky protein that promotes pancreatic cancer. The problem is getting the drug into the tumor, or even anywhere near the pancreas.
“Unfortunately, this drug cannot reach the pancreas, because the bones absorb up to 90% of it immediately,” explains Sushanta. “It has high bone absorption.”
Enter the nanoparticle being developed by the Kansas City team and their collaborators to the north. It’s a tiny chemical package that carries zoledronic acid inside, along with a peptide—a chain of amino acids—called iRGD, which has a strong affinity for cancer cells and acts as a homing molecule.
The combination is wrapped in a polymer that opens only under certain conditions—namely, an environment that is very low PH, or very acidic, and hypoxic, meaning there is very little oxygen. Because of desmoplasia, the buildup of scar tissue, that’s precisely what it’s like inside a pancreatic tumor.
“We inject this nanoparticle into mice and it enters only into the tumor cells,” says Sushanta.
“Then it opens up and releases the drug. It will not go anywhere else in the body, only into cancer cells, and it will open only in a hypoxic condition.”
“We found that bone absorption is zero,” he notes.
From a clinical perspective, Kambhampati, the oncologist, says that “zoledronic acid is very relevant because it’s already being used in pancreatic cancer patients, although mostly to address the bone symptoms and high calcium levels.” In other words, doctors already have a good idea of the drug’s overall safety and tolerability in those with cancer.
He likes that the nano approach addresses “the key challenge that remains in pancreatic cancer—tumor impermeability.”
Asked whether he thinks the nanoparticle method using zoledronic acid will be an option for patients in a few years, he says, “It’s very promising.”
VA Research Currents archives || Sign up for VA Research updates